Neurostimulation Systems Are Showing Promise
WASHINGTON, DC — The last decade has seen health systems the world over shift away from using opioids for pain management. First, there was the too-slow understanding that opioids are addictive and were being massively over-prescribed. Later came studies showing that opioids, while providing short-term relief, are ineffective for long-term pain management. Patients and physicians have been left scrambling to find an opioid alternative for chronic pain.
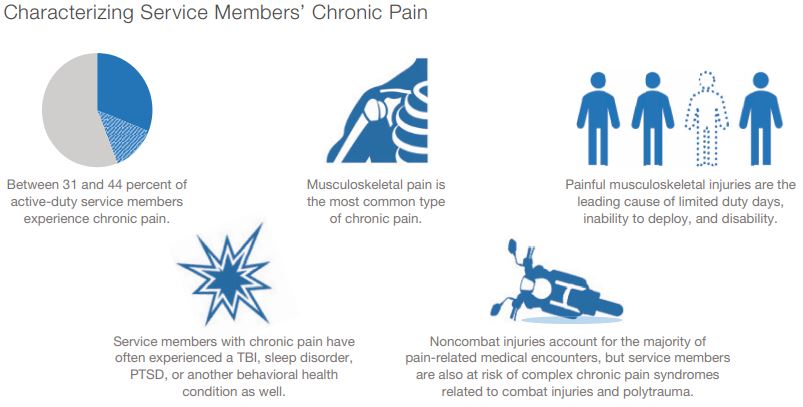
This is especially true in VA and DoD, whose patient populations suffer from chronic pain at a higher rate than others without military service. According to the national Centers for Disease Control and Prevention, active-duty servicemembers suffer from chronic pain at a rate about 1.5 to 2-times higher (31-40%) than the general population (20%). As many as 40% of veterans who were deployed in Iraq and Afghanistan suffer from some combination of chronic pain, PTSD and TBI.
This has profound effects on patients’ quality of life, as well as on the state of the military as a whole. According to a RAND study published last year, chronic pain is the leading cause of disability and reduced readiness in the military.1
The most common type of pain among servicemembers is musculoskeletal pain, particularly back and joint disorders. Chronic pain also is more common for injured veterans or those exposed to high-intensity combat.
“Because of the unique occupational exposures associated with deployments … servicemembers also are at risk of more complex chronic pain syndromes,” the report states. “For example, combat injuries, particularly blast injuries, can result in complex polytrauma, with a higher number, severity, and diversity of wounds and a high incidence of concurrent traumatic brain injury.”
However, combat is not necessary for servicemembers to experience debilitating pain. A study of U.S. Army personnel data cited in the RAND report suggests that noncombat musculoskeletal injuries account for almost 60% of soldiers’ limited duty days and 65% of soldiers who are medically unable to deploy. Also, these injuries are the leading cause of hospitalization and disability among servicemembers, accounting for 40-50% of DoD disability benefits payments.
To care for these patients, VA and DoD are trying everything from centuries-old techniques to cutting-edge technology. Treatments include physical therapy, occupational therapy, chiropractic treatment, cognitive behavioral therapy, as well as other alternative therapies such as acupuncture. On the medication front, physicians have moved from away from opioids and towards NSAIDs, anticonvulsants, antidepressants, and muscle relaxants in an attempt to ease patients’ pain.
However, studies have shown that the effectiveness of these medications is limited, especially for lower back pain—a very common complaint among servicemembers and veterans—and there are hazards if used for long periods of time.
A study published in 2015 in the British Medical Journal found that acetaminophen is ineffective in the treatment of low back pain and that those who use it are four times more likely to have abnormal results on liver function tests.2
Other studies have found NSAIDs slightly more effective than placebo over the short term. But side effects of long-term use and adverse interactions with other common medications may rule out NSAIDs for many patients.
Spinal-Cord Stimulators
One promising avenue of care that has increased over the past two decades is the use of spinal-cord implants to treat lower back pain. A study published in 2020 in the Journal of Pain Research looked at 1,490 veterans who had received spinal-cord stimulator (SCS) implants between 2000 and 2012. Over 90% of those receiving an SCS had been prescribed opioids during the year prior to their implant.3
Veterans who had a pre-surgical pain score greater than 4 experienced a clinically significant decrease in pain after implantation. There also was a significant decrease in patients receiving opioid therapy (92% to 86%) and a significant decrease in the opioid dose.
“Serious concerns have been raised about the escalating rates of adverse health consequences from long-term opioid therapy, including overdose and death,” the study’s authors note. “It is particularly important for veterans with chronic pain to have access to additional pain management strategies, such as SCSs, that can help manage pain.”
A more recent study on spinal-cord stimulation published last January in the Federal Practitioner found that 77% of veterans would recommend SCS to their peers, and that patients reported a statistical difference in 16 of 18 categories of activities of daily living.4
“For veterans with chronic intractable pain who have tried and failed more conservative treatments, SCS is a great treatment,” the study’s authors declared.
Many of these studies note that research examining treatments for chronic lower back pain is lacking, despite its high prevalence among veterans and servicemembers. The RAND report noted the same discrepancy, finding that, while treatment options are increasing, there is still much that is not known about effective treatment of chronic pain, especially in the military.
“Few studies have examined the extent to which evidence-based non-pharmacologic therapy, multimodal pain treatment, multidisciplinary team-based care, and stepped care are used to manage chronic pain,” the researchers note in the report. “Research to address these gaps in the evidence base could guide efforts by the MHS to improve the quality of chronic pain care, as well as inform DoD’s investments in chronic pain research and clinical interventions.”
- Sherry, TB, Roth CP, Bhandarkar M, Hepner K. Chronic Pain Among Service Members: Using Administrative Data to Strengthen Research and Quality Improvement. Santa Monica, CA: RAND Corp., 2021. https://www.rand.org/pubs/research_reports/RRA1160-1.html.
- Machado GC, Maher CG, Ferreira PH, Pinheiro MB, Lin CW, Day RO, McLachlan AJ, Ferreira ML. Efficacy and safety of paracetamol for spinal pain and osteoarthritis: systematic review and meta-analysis of randomised placebo controlled trials. BMJ. 2015 Mar 31;350:h1225. doi: 10.1136/bmj.h1225. PMID: 25828856; PMCID: PMC4381278.
- Wandner LD, Fenton BT, Goulet JL, et al. Treatment of a Large Cohort of Veterans Experiencing Musculoskeletal Disorders with Spinal Cord Stimulation in the Veterans Health Administration: Veteran Characteristics and Outcomes. J Pain Res. 2020;13:1687-1697. Published 2020 Jul 7. doi:10.2147/JPR.S241567
- Murphy CA, Roig RL, Trimble WB, Bennett M, Doughty J. Review of Efficacy and Safety of Spinal Cord Stimulation in Veterans. Fed Pract. 2022 Jan;39(1):32-36a. doi: 10.12788/fp.0204. Epub 2022 Jan 12. PMID: 35185318; PMCID: PMC8849029.