WASHINGTON, DC — Veterans who use dual systems (i.e., both VA and non-VA services, for medical care) are more likely to receive a new opioid prescription and to receive a diagnosis of opioid use disorder, according to a recent study.
The retrospective cohort study published in the journal Frontiers in Public Health examined whether dual-system use was associated with increased rates of new opioid prescriptions, continued opioid prescriptions and diagnoses of opioid-use disorder. Dual-system use was defined as receipt of VA care and VA payment for non-VA services. Mono users were those who only received VA services. The researchers hypothesized that dual-system use would be associated with increases in each category.1
“The prevalence of opioid prescriptions has been declining in the U.S. healthcare systems including VA, yet the prevalence of OUD has not been declining at the same rate,” wrote researchers from the VA Connecticut Healthcare System in West Haven and the Yale School of Medicine in New Haven, CT, and colleagues. “One potential problem is that detailed notes from non-VA visits are not immediately available to VA clinicians, and information about VA care is not readily available to non-VA sources. One implication of our findings is that better health system coordination is needed. Even though care was paid for by the VA and presumably closely monitored, dual-system users were more likely to have new and continued opioid prescriptions.”
When patients access multiple opioid prescription sources, efforts to achieve opioid guideline-concordant care might be undermined, the authors suggested, adding that their research was conducted because no prior studies have examined the impact of dual-system use of VA services and VA-paid community care on opioid safety outcomes.
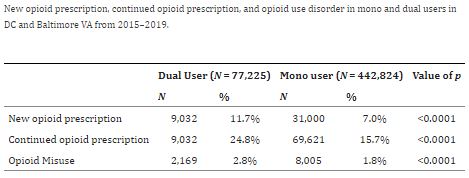
The study used VA data from two facilities, the Washington, DC, and Baltimore VAMCs, from 2015 to 2019 and included active veteran patients who had at least one encounter in a calendar year during the 4-year period. There were 77,225 dual-system users and 442,824 mono users. Three outcomes were measured: new opioid prescription, continued opioid prescription (i.e., received an additional opioid prescription) and diagnosis of opioid use disorder (during the calendar year).
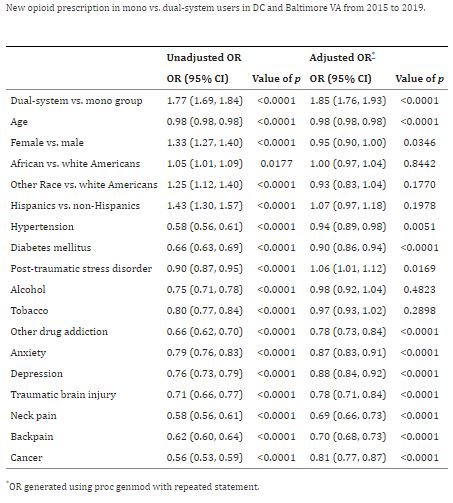
The study found that dual-system users were significantly younger than mono users, more likely to be women and less likely to report white race. Results indicated that dual-system users were significantly more likely to receive a new opioid prescription during the observation period [Odds ratio (OR) = 1.85, 95% confidence interval (CI) 1.76-1.93], continue prescriptions (OR = 1.24, CI 1.22–1.27), and to receive an opioid-use disorder diagnosis (OR = 1.20, CI 1.14-1.27).
New opioid prescription was defined as no opioid prescription in the VA prior to the opioid prescription in the current calendar year. Continued opioid prescription was defined as the receipt of any opioid prescriptions in the current calendar year and having prior prescriptions. Opioid medications included codeine, fentanyl, hydrocodone, hydromorphone, levorphanol, meperidine, morphine, oxycodone, oxymorphone, pentazocine, tapentadol and tramadol. Buprenorphine and methadone were excluded, because most of their use is to treat opioid-use disorder.
Prescribing Guidelines
To promote safer opioid use and decrease opioid mortality, health systems, including the VA, have developed opioid prescribing guidelines, which include recommendations for providers to avoid prescribing opioids for the treatment of chronic pain. If prescribing opioids, providers should check prescription drug-monitoring databases for evidence of other controlled substances prescriptions from other prescribers and implement opioid-risk-mitigation strategies. The authors expressed concern that fragmented care from multiple opioid prescription sources is associated with high-risk prescribing practices and opioid-use disorder. That can be exacerbated by lack of shared information, they added.
The VA is considered to be in a unique situation, because many of its patients are dual-system users who receive care at the VA, as well as access community care that may be paid for by the VA. “The community care that VA pays for through VCP/VCCP brings an additional layer of responsibility for VA to understand the impact of dual-system use, especially as it may impact opioid safety, yet no prior studies have examined the impact of dual-system use of VA service and VA paid community care on opioid safety outcomes,” the authors noted.
After adjusting for demographic factors and comorbid conditions, the analysis found that dual-system users receive more opioid prescriptions and exhibit more OUD than mono users. “In addition, the associations of demographic and clinical factors with new opioid prescription initiation and use differed among the VA mono and dual-system user groups in important ways,” the researchers pointed out. “Younger and female veterans are slightly less likely to receive opioid prescriptions. Female, Hispanic, and other race veterans are much less likely to have an OUD diagnosis.”
“One implication of our findings is that health system coordination is important,” the study authors noted in response to questions from U.S. Medicine. “In particular, in regard to opioid prescribing, processes such as querying prescription drug monitoring programs are important tools to facilitate awareness and coordination across systems.”
A limitation of the study was that the dual-system user category was limited to the Veteran Choice Program and Veterans Community Care Program. Many veterans have private insurance, and these programs are only a subset of the dual-system users.
“We at VA will stop at nothing to get veterans who live with substance use disorder the help they need and deserve,” the study authors wrote in an email. “VA offers a comprehensive continuum of specialty substance use disorder (SUD) services for veterans, not just medication-based treatment. This continuum of care includes specialty SUD treatment outpatient and residential programs. It also includes treatment and engagement outside of SUD specialty settings, with a focus on engaging veterans where they are most likely to present for care (e.g., primary care, pain management and general psychiatry clinics).”
- Goulet J, Cheng Y, Becker W, Brandt C, Sandbrink F, Workman TE, Ma P, Libin A, Shara N, Spevak C, Kupersmith J, Zeng-Treitler Q. Opioid use and opioid use disorder in mono and dual-system users of veteran affairs medical centers. Front Public Health. 2023 Apr 4;11:1148189. doi: 10.3389/fpubh.2023.1148189. PMID: 37124766; PMCID: PMC10141670.