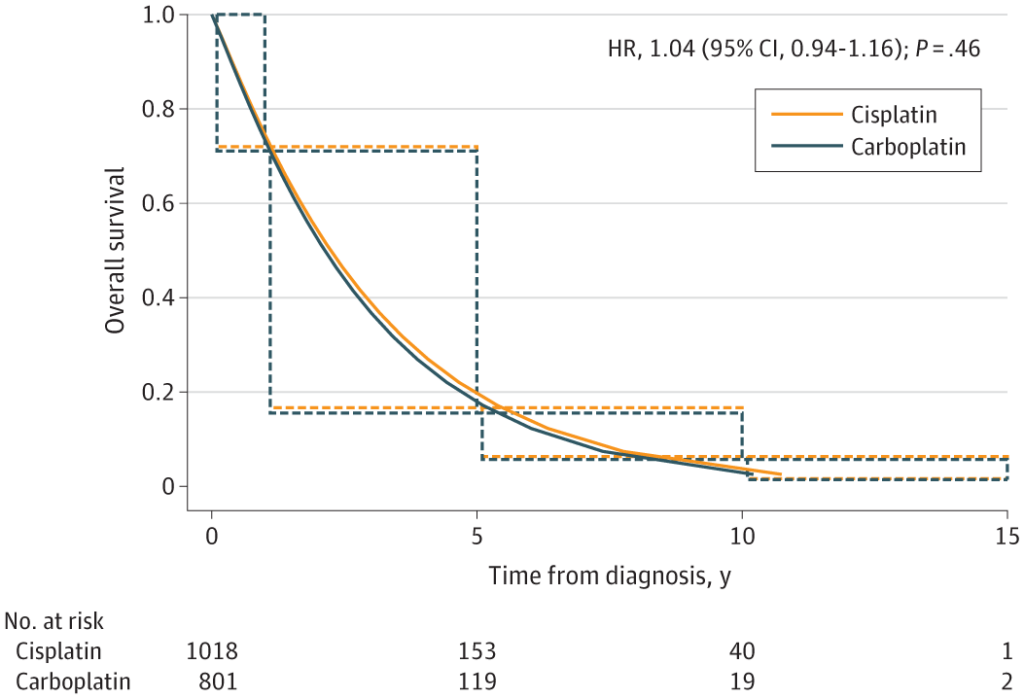
Click to Enlarge: The solid lines were estimated by a parametric Weibull proportional hazards regression analysis for interval censored data, and the dotted lines were generated by an interval-censored Cox proportional hazard model. HR indicates hazard ratio. Source: JAMA Network Open
DETROIT — Lung cancer is the third-most-common form of cancer and the leading cause of cancer mortality in the U.S. Because of their high rate of smoking and, potentially, military-related exposures, veterans are at greater risk of lung cancer than the general population. Thus, determining the most effective lung cancer treatments is a priority of VA research.
Two recent studies led by Ibrahim Azar, MD, a hematology and oncology resident at Karmanos Cancer Institute, Wayne State University School of Medicine, in Detroit, provided new insight into the effectiveness of widely used treatments for small cell lung cancer (SCLC), which comprises 10% to 15% of cancer diagnoses in veterans.
In a new study published in Clinical Lung Cancer, Azar and his colleagues found that treatment including surgery was associated with longer overall survival compared to chemoradiotherapy (CRT), which historically been the treatment for limited stage small cell lung cancer.
While current National Comprehensive Cancer Network (NCCN) guidelines recommend consideration of lobectomy in node-negative cT1-T2 SCLC, data regarding the role of surgery in very limited SCLC is lacking, Azar and his colleagues wrote. To better understand that role the researchers collected data of patients with stage 1 SCLC from the National VA Cancer Care Cube Registry. Only 661 patients that had either received surgery or concurrent CRT were included. Of these, 446 patients had received concurrent CRT; while 223 underwent treatment that contained surgery (93 surgery only, 87 surgery/chemo, 39 surgery/chemo/radiation and 4 surgery/radiation). The median overall survival for the surgery-inclusive treatment was 3.87 years, while median overall survival for the CRT cohort was 2.45 years, they found. Subset analysis based on the location of the tumor in both the upper or lower lobes showed improved survival with surgery as compared to CRT regardless of the location.1
In an earlier study, published in JAMA Network Open, Azar and his colleagues compared two platinum-based drugs, carboplatin and cisplatin, the backbone of chemotherapy for limited-stage SCLC (LS-SCLC) and extensive-stage SCLC (ES-SCLC), they wrote.
“We knew from prior studies and meta-analyses that the use of carboplatin and cisplatin in extensive stage SCLC was associated with similar overall survival,” said Azar. “Prior to our study, the prevailing thought was that, in limited stage SCLC, where the goal is cure, cisplatin is the agent to use. However, there are no trials comparing the two.”
To compare the two agents head to head, the researchers examined data from the National Veterans Affairs Central Cancer Registry for patients with SCLC who received platinum-based multiagent chemotherapy between 2000 and 2020 for ES-SCLC and 2000 and 2021 for LS-SCLC. Only patients with pathologically confirmed cases of LS-SCLC who received concurrent chemoradiation and ES-SCLC who received chemotherapy were included.
Among 2,652 patients with ES-SCLC, 2032 were treated with carboplatin-based therapy and 660 received cisplatin; the median overall survival was 8.45 for cisplatin and 8.51 months for carboplatin. Subset analysis showed no survival difference between the two agents in different age or performance status groups except for patients aged 70 years and older, for whom the median overall survival was 6.36 months for carboplatin.2
Of 1,756 patients with LS-SCLC, 801 received carboplatin and 1,018 received cisplatin. The median overall survival was 26.92 months for cisplatin and 25.58 months for carboplatin. The median overall survival was not significantly different between two agents according to cancer stage (I-III), performance status and age groups. A multivariable analysis of factors associated with overall survival accounting for stage (I-III), performance status and age did not demonstrate a significant difference in survival between carboplatin and cisplatin in patients with LS-SCLC, they wrote.
Because veterans tend to have a significant number of co-morbidities, choosing the less toxic agents in SCLC is very important, said Azar. Cisplatin carries great toxicity to kidneys, nerves, hearing and a higher risk of nausea and vomiting, he said.
“Our study showed no difference in overall survival between carboplatin and cisplatin in either extensive stage or limited stage SCLC,” Azar said. “While most oncologists use carboplatin for ES-SCLC, cisplatin is currently preferred by guidelines and most practitioners in LS-SCLC. Our study challenges the notion of superiority of cisplatin in LS-SCLC and opens the door to future randomized clinical trials to answer this question.”
“Importantly,” he added, “there is currently a national shortage of platinum agents of both carboplatin and cisplatin that has significantly affected oncologists and their day-to-day practice. Oncologists should feel comfortable substituting cisplatin for carboplatin in limited stage SCLC, especially if cisplatin is in short supply.”
- Azar I, Austin A, Saha BK, Kim S, Jang H, Sbihi AA, Alkassis S, Yazpandanah O, Chi J, Dhillon V, Mehta HJ, Chopra A, Neu K, Mehdi SA, Mamdani H. The Role of Surgery in Stage I Small Cell Lung Cancer: A National VA Database Analysis. Clin Lung Cancer. 2023 Jul;24(5):e179-e186. doi: 10.1016/j.cllc.2023.04.002. Epub 2023 Apr 15. PMID: 37217388.
- Azar I, Yazdanpanah O, Jang H, Austin A, Kim S, Chi J, Alkassis S, Saha BK, Chopra A, Neu K, Mehdi S, Mamdani H. Comparison of Carboplatin With Cisplatin in Small Cell Lung Cancer in US Veterans. JAMA Netw Open. 2022 Oct 3;5(10):e2237699. doi: 10.1001/jamanetworkopen.2022.37699. Erratum in: JAMA Netw Open. 2023 Jan 3;6(1):e2246257. PMID: 36264573; PMCID: PMC9585434.
