Rates for Breast, Cervical, Colorectal Cancer Aren’t High, However
SEATTLE — Low-value healthcare is defined as practices or procedures without clear benefit or where potential harm outweighs the benefit. Deciding what is and isn’t low-value care can be especially difficult when it comes to cancer screenings; increasing age, greater illness burden or lower life expectancy—all weigh on decision-making.
A new study finding that low-value prostate cancer screenings are common in the VHA has raised questions about how well clinicians are walking that tightrope. In some cases, for example, procedural complications or testing burden outweigh the expected benefits from detecting slow-growing cancers.
The recent cohort study led by VA Puget Sound Health Care System researchers looked at the care of nearly six million veterans, finding that fewer than 3% of cancer screening recipients received a low-value test for breast, cervical or colorectal cancer. At the same time, however, 39% of men screened for prostate cancer were considered to have received a low-value test.
The report in JAMA Network Open added that no single factor—whether patient, clinician, clinical or organizational characteristic—was linked to a greater likelihood of using low-value screening receipt across four cancer types.
“Most clinical practice guidelines recommend stopping cancer screenings when risks exceed benefits, yet low-value screenings persist,” the authors wrote. “The Veterans Health Administration focuses on improving the value and quality of care, using a patient-centered medical home model that may affect cancer screening behavior.”
The study team sought to understand rates and factors associated with outpatient low-value cancer screenings by focusing on the care of .patients with cancer screenings in 2017 at VHA primary care clinics. Participants, 91.7% men, had a mean age of 63.1 and most, 75.7%, were white. Analysis of data occurred from Dec. 23, 2019, to June 21, 2021.
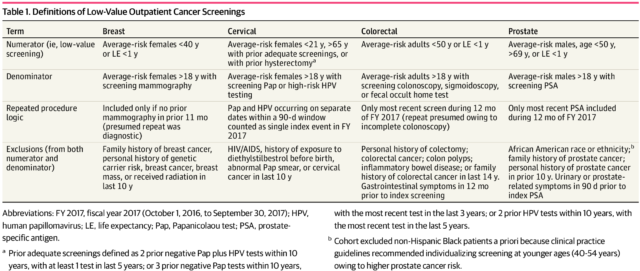
For purposes of the study, low-value screenings were defined as those occurring for average-risk patients outside of guideline-recommended ages or if the one-year mortality risk estimated using a previously validated score was at least 50%.
Researchers determined that 19.4% of men of average risk underwent prostate cancer screening; 5.2% of patients underwent colorectal cancer screening; 4.7% of 469,045 women of average risk underwent breast cancer screening; and 14.3% of 458,086 women of average risk underwent cervical cancer screening.
“Of patients screened, low-value testing was rare for three cancers, with receipt of a low-value test in 633 of 21,930 of women screened for breast cancer (2.9%), 630 of 65,511 of women screened for cervical cancer (1.0%), and 6,790 of 299,765 of patients screened for colorectal cancer (2.3%),” the authors advised. “However, 350,705 of 4,647,479 of screened men (7.5%) received a low-value prostate cancer test.”
They added, “Patient race and ethnicity, sociodemographic factors, and illness burden were significantly associated with likelihood of receipt of low-value tests among screened patients. No single patient-, clinician-, or clinic-level factor explained the receipt of a low-value test across cancer screening cohorts.”
Overall, the large cohort study determined that low-value breast, cervical and colorectal cancer screenings were rare at the VHA. Yet, they also documented that testing of more than one-third of patients screened for prostate cancer were outside of clinical practice guidelines. “Guideline-discordant care has quality implications and is not consistently explained by associated multilevel factors,” the researchers noted.
The study pointed out that many clinical practice and organizational guidelines recommend stopping cancer screenings when life expectancy falls below a certain threshold, such as 10 years. Still, despite guidelines and relative risks, the authors recounted how more than 50% of adults with reduced life expectancy report ongoing cancer screening.
The practice also comes with a cost, they emphasized, with Medicare having spent $790 million on guideline-discordant prostate, cervical and colon cancer tests in 2009.
While there are many explanations about how inappropriate screening occurs, “it is unclear how multilevel factors are associated with low-value cancer screenings, particularly within an integrated health system with salaried clinicians, such as the Veterans Health Administration (VHA),” the authors wrote.
The study described how VHA uses a multidisciplinary patient-centered medical home (PCMH) model in more than 900 clinics. The model, which emphasizes teamwork, population health management, continuity and care quality, has increased the capacity for preventive screenings with use of care registries, expanded staffing and dedicated infrastructure.
“Although PCMH models have been associated with improved preventative care delivery, connections to low-value cancer screenings have not been examined,” the researchers advised. “Paradoxically, more low-value screenings could occur with expanded access or protocolized screenings delivered via enhanced team structures. Alternatively, low-value cancer screenings may decrease with greater clinician continuity from PCMH implementation; another study found that continuity was associated with fewer low-value tests.”
The authors suggested that gaining more understanding of how low-value screenings are associated with PCMH organizational characteristics could help with future intervention design or implementation strategies.
“Our study is among the first to operationalize validated recommendations for low-value testing among common cancer screenings and to examine associations with multilevel factors for the VHA,” the authors wrote. “Overall, testing for breast, colorectal or cervical cancer was rarely low value, among both all average-risk patients or screening recipients. However, low-value prostate cancer tests were more common, received by 7.6% of all average-risk men and 38.8% of screened men. Predominantly patient factors were associated with higher likelihood of receipt of low-value cancer testing among screened patients; however, no single factor was significant in one direction across all 4 cohorts. There was also no clear association between select domains of the VHA PCMH model and low-value test receipt.”
The study pointed out that the integrated system of the VHA could attract different patient populations and result in more variation in screening activities because of equitable access, informational continuity, fewer financial barriers to care or fewer incentives for services compared with other systems.
Screening Disparities
While some community healthcare systems have cancer screening disparities, “racial and ethnic minority populations have greater parity in the VHA and the U.S. Department of Defense health care systems. Patient race and ethnicity, illness burden, and copay status were significantly associated with likelihood of low-value test receipt across cancer screening cohorts, but the direction of association differed.”
With higher rates of low-value testing for prostate cancer, the researchers said they posited at one point that persistent testing outside guidelines may be associated with history of Vietnam-era Agent Orange exposure, a risk factor for prostate cancer but saw no evidence for that in subgroup analysis.
“While in aggregate, low-value cancer screenings may pose greater risk than benefit, testing outside established recommendations must be individualized, as algorithmic decisions may misclassify patients otherwise appropriate for screening,” the authors explained. “Clinicians should engage in shared decision-making with those patients. Communication strategies, decision aides, and conceptual frameworks for these challenging conversations have been proposed, supported by the American Cancer Society and the U.S. Preventive Services Task Force.”
They also called for the development of better predictions for which patients might benefit from screenings, beyond chronological age, writing, “Individualized recommendations for cancer screening may help to advance care quality, particularly for patients with advanced age or poor health status.”
- Schuttner L, Haraldsson B, Maynard C, et al. Factors Associated With Low-Value Cancer Screenings in the Veterans Health Administration. JAMA Netw Open. 2021;4(10):e2130581. doi:10.1001/jamanetworkopen.2021.30581