WASHINGTON, DC — Nearly all patients hospitalized for acute heart failure are acutely congested due to fluid retention and have gained weight by the time of their admission. As a result, diuretics are commonly prescribed for fluid removal; evidence shows that the use of powerful loop diuretics is associated with improved clinical outcomes in heart failure patients.
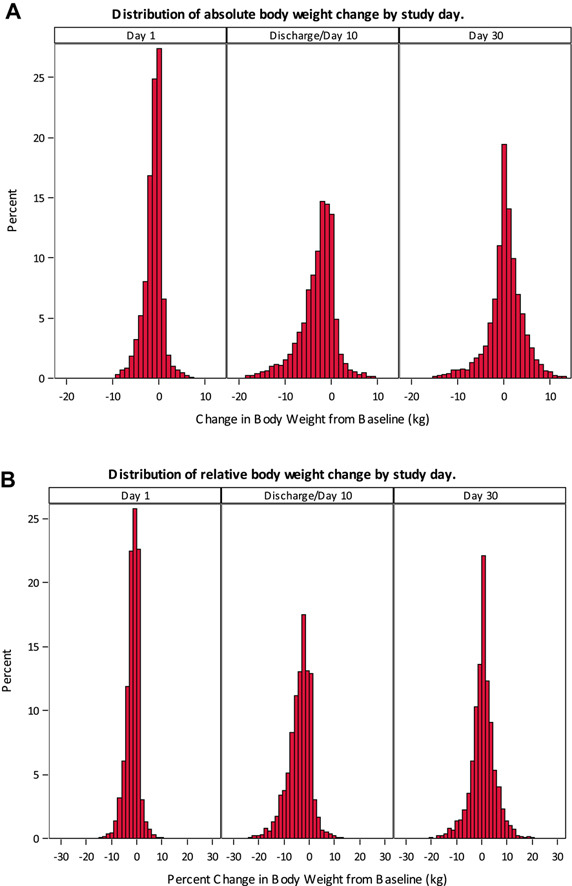
Successful decongestion is often associated with weight loss, and in-hospital changes in weight have been historically used as a sign that diuretics are effective. Limited data exists, however, on whether weight loss itself is associated with improved outcomes. A new analysis by researchers at the Washington, DC, VAMC sought to shed more light on the connection between in-hospital weight loss and patient outcomes.1
The researchers used data from the national Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients With Heart Failure (OPTIMIZE-HF) registry, which was based on more than 48,000 hospitalizations with a code of heart failure as the primary discharge diagnosis between March 1, 2003, and Dec. 31, 2004. After linking the registry data to Medicare data and excluding patients with missing weight, dialysis, weight gain of more than 1 kilogram and weight loss of more than 30 kilograms, 16,060 patients with heart failure remained in the study cohort.
The analysis, which was published in The Journal of Cardiac Failure, found that patients who lost weight had a lower risk of hospital readmission for heart failure and a lower risk of all-cause mortality compared with those who did not lose weight, and these associations remained significant up to 60 days post-discharge. Those patients were also less likely to be referred to hospice care. (However, weight loss was not associated with a lower risk of being discharged to in-home healthcare or a nursing home.)
“We have previously demonstrated that the use of diuretics was associated with improved clinical outcomes in patients hospitalized with heart failure, which were more pronounced in patients with evidence of significant congestion,” said senior author Ali Ahmed, MD, MPH, associate chief of staff for health and aging at the DCVAMC and professor of medicine at George Washington University. “Therefore, it did not come as a complete surprise to us that weight loss, which is considered a surrogate for successful decongestion in the acute setting, was associated with improved outcomes.”
The study authors noted that the most plausible explanation for weight loss is the use of diuretics, although the reasons for lack of weight loss may be multifactorial. In some cases, patients might be resistant to diuretic medications. In other cases, the lack of weight loss may also be attributable to the use of lower doses or frequency of diuretics.
“The early rise of serum creatinine in response to diuretic use may be perceived as a worsening kidney function, discouraging a dose escalation necessary to achieve diuresis and fluid removal,” said the paper’s lead author Phillip H. Lam, M.D., assistant professor of medicine at Georgetown University and an advanced heart failure and transplant cardiologist at the MedStar Heart & Vascular Institute at MedStar Washington Hospital Center and the Washington D.C. VA Medical Center.
The findings contrast to those of a prior trial, the Acute Study of Clinical Effectiveness of Nesiritide and Decompensated Heart Failure (ASCEND-HF), which found that weight loss was not associated with improved outcomes in relatively younger patients in the trial.2
“Most heart failure patients are older adults. Patients in the ASCEND-HF were younger patients with a mean age of 65, plus or minus 14 years,” said Ahmed. “In contrast, real-world patients in our study had a mean age of 78, plus or minus 10 years. So, the findings of our study are more generalizable to real-world hospitalized heart failure patients.”
However, he notes, there is no reason to believe that weight loss is associated with better outcomes only in older patients. “The lack of a significant association between weight loss and better outcomes in ASCEND-HF is also likely due to methodological differences between these two studies.”
Although the analysis did not include veterans (OPTIMIZE-HF had enrolled veterans but they were excluded during the linking process with Medicare data), the study authors suggested the results should be generalizable to veterans with heart failure who are hospitalized in VA medical centers.
“Patients with acute heart failure, veterans or nonveterans, are congested with fluid retention and are treated with diuretics that result in fluid removal and decongestion,” said study co-author Gregg C. Fonarow, MD, professor of medicine and director of the Division of Cardiology at the University of California-Los Angeles. “Thus, weight loss due to successful diuresis would be expected to have a similar association in nearly all hospitalized heart failure patients.”
The study’s findings showed that weight is an important vital sign in patients with heart failure, the authors say. Acute changes in weight over short periods have been used by clinicians to monitor fluid retention, guide diuretic therapy and assess response to diuresis. This analysis suggested that weight loss, a biomarker for effective in-hospital diuresis, is also associated with improved clinical outcomes. Still, they noted, future studies need to examine whether other interventions, such as more aggressive diuresis and ultrafiltration, may improve outcomes in hospitalized heart failure patients who fail to lose weight in response to diuretic therapy.
- Gauravpal, GS.; Lam, PH; Brar, V; Morgan, C; Fonarow, GC.; Ahmed, A.. In-Hospital Weight Loss and Outcomes in Patients With Heart Failure. Journal of Cardiac Failure. Published December 23, 2021. DOI: 10.1016/j.cardfail.2021.11.017
- Ambrosy AP.; Cerbin, LP; Armstrong, PW; Butler, J. et. al. aved; Coles, Adrian; DeVore, Adam D.; et al. Body Weight Change During and After Hospitalization for Acute Heart Failure: Patient Characteristics, Markers of Congestion, and Outcomes: Findings From the ASCEND-HF Trial. Journal of the American College of Cardiology (JACC): Heart Failure. Published January 2017. DOI: 10.1016/j.jchf.2016.09.012.