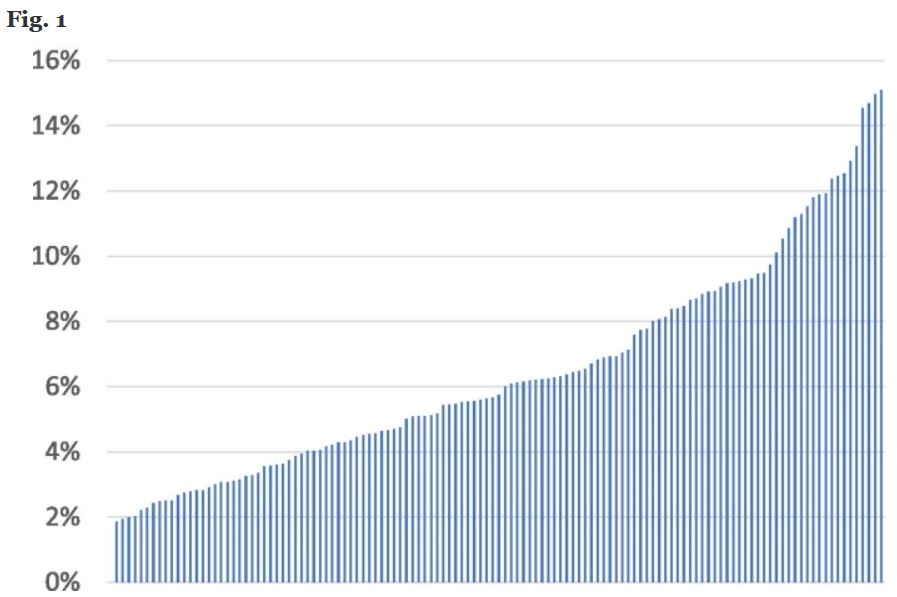
Click To Enlarge: Site-variation in guideline-discordant DOAC prescribing, 2010–2016. Includes prescriptions for dabigatran, rivaroxaban, and apixaban. Proportion of patients appropriate for full-dose DOAC therapy who received low-dose therapy instead, by site. Among 126 sites with at least 100 patients in the denominator
WASHINGTON, DC — Since they were first approved by the Food and Drug Administration in 2010, direct-acting oral anticoagulants (DOACs) have become the most commonly-prescribed anticoagulants for nonvalvular atrial fibrillation (NVAF) due to their predictable pharmacokinetics, few drug-drug interactions and low monitoring requirements.
Yet, although clear guidelines exist to guide their dosing, a new study found a substantial portion of DOAC prescriptions in the VA healthcare system are dosed contrary to those guidelines.
To understand the consistency with which DOAC prescribing guidelines are followed in clinical practice, researchers led by Adam Rose, MD, associate professor, Hebrew University School of Public Health in Jerusalem, studied VA NVAF patients who received DOACs—dabigatran, rivaroxaban or apixaban—between 2010 and 2016. The researchers used patient characteristics (age, creatinine, body mass) to identify which patients met FDA and VA guideline recommendations for low-dose therapy and which for full-dose therapy. 1
Included were 73,672 veteran who were prescribed DOACS. Of 5,837 patients who were recommended to receive low-dose therapy, 1,331 (23%) received full-dose therapy instead. Of 67,935 patients recommended receiving full-dose therapy, 4,079 (6%) received low-dose therapy instead.
The researchers reported in BMC Health Services Research that VA sites varied widely in terms of how often guideline-discordant dosing occurred. On inappropriate low-dose therapy, sites varied from 0 to 15%, while on inappropriate high-dose therapy, from 0 to 41%.
Guideline-discordant therapy decreased by about 20% in a relative sense over time, but its absolute numbers grew as DOAC therapy became more common, the authors reported. The most important patient-level predictors of receiving guideline-discordant therapy were older age and creatinine function being near the cutoff value.
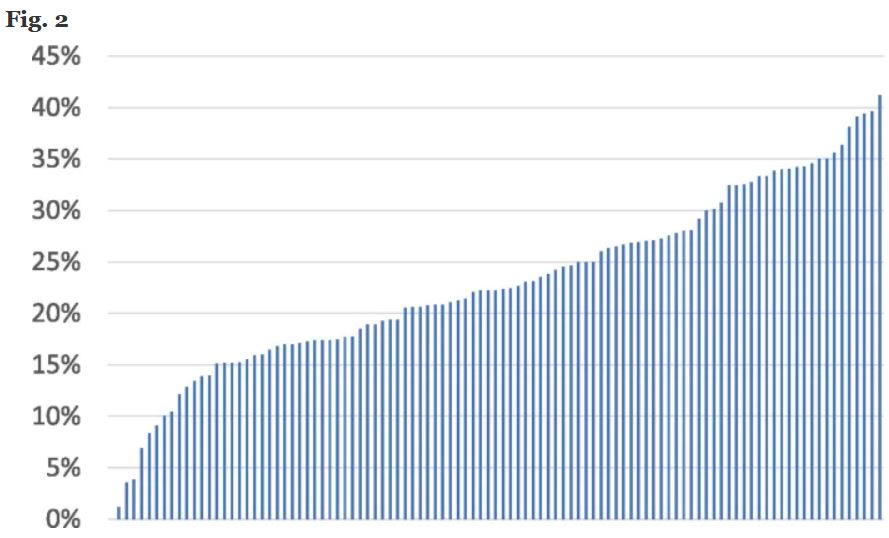
Click To Enlarge: Site-variation in guideline-discordant DOAC prescribing, 2010–2016. Includes prescriptions for dabigatran, rivaroxaban, and apixaban. Proportion of patients appropriate for low-dose DOAC therapy who received full-dose therapy instead, by site. Among 103 sites with at least 20 patients in the denominator
Rose said he was not surprised by the disconcordance. “This is not a new finding in some ways.” he said. “With warfarin, the older anticoagulant, many physicians tried to be smarter than the guidelines and tried to underdose patients, thinking that they could minimize the risk of bleeding,” he said. “People are naturally scared of errors of commission—as enshrined in the adage, ‘first do no harm’—but evidence-based medicine dictates that you should use the dose that was proven to work, not try to be smarter than the evidence. It’s true here as well.”
He added that the variation among sites speaks to local practice patterns, but also to the levels of control and oversight at some VA facilities versus others. Overall, however, he suggested that the discordance he and his colleagues found at the VA is likely to be lower than that in other healthcare systems and that, importantly, the VA is in a better position than other health systems to correct it.
“VA usually does better than other systems in this regard, because VA has clear guidelines and centralized mechanisms of control and oversight, which other systems often lack,” he said. “Even with all the guideline-discordant therapy we saw in this study, I’m sure the way the VA is ‘built’ to cut down on it quite a lot, and we would have seen even more of it in a less coherent health system.”
Now that the magnitude of guideline-discordant prescribing has been documented, Rose said it’s important to better understand and address the issue. “The next logical step would be an in-depth analysis of why this happens, followed by planning a logical intervention on those findings.”
Such interventions would likely be targeted at the VA’s systems rather than the providers, who don’t always follow the guidelines. “It’s easy to blame providers, but really we need better systems,” he said. “If it was built into the VA’s computer system that guideline-discordant doses need to be justified or else won’t be filled, there would be a lot less of it happening.
“Your system will always be inhabited by human beings,” he added. “But airplanes don’t crash all the time—even though they are piloted by humans—because there are redundant systems to prevent error. We can have that here too.”
- Rose AJ, Lee JS, Berlowitz DR, Liu W, Mitra A, Yu H. Guideline-discordant dosing of direct-acting oral anticoagulants in the veterans health administration. BMC Health Serv Res. 2021 Dec 18;21(1):1351. doi: 10.1186/s12913-021-07397-x. PMID: 34922546; PMCID: PMC8684634.

