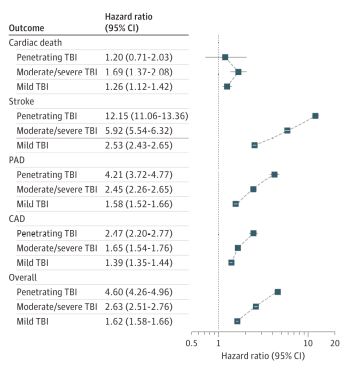
Click to Enlarge: Hazard Ratio and 95% CIs for the Individual and Composite Outcomes in Fully Adjusted Models Stratified by Traumatic Brain Injury (TBI)CAD indicates coronary artery disease; PAD, peripheral artery disease. Source: JAMA Neurology
BETHESDA, MD — Traumatic brain injury (TBI) was common among U.S. servicemembers deployed to Iraq and Afghanistan, with up to 20% sustaining at least one TBI. Although the survival rate for such injury was high, research has suggested TBI is associated with a wide variety of adverse effects, including dementia, epilepsy and mental health conditions.
This risk has concerned researchers, including Air Force Lt. Col. Ian J. Stewart, MD, of Uniformed Services University, who led a new study examining an association between traumatic brain injury and another health problem in post-9/11-era veterans—cardiovascular disease.1
“Although heart disease and stroke are the leading and fifth most common causes of death in the U.S., respectively, there are few studies that examine TBI as a risk factor for cardiovascular disease,” Stewart and his colleagues wrote in JAMA Neurology. “Prior work has demonstrated associations between TBI and both hemorrhagic and ischemic stroke. However, these studies examined older, civilian populations and may not be generalizable to post-9/11-era veterans.”
The new retrospective cohort study, which examined a more comprehensive definition of cardiovascular disease in the younger veteran population, was conducted from Oct. 1, 1999, to Sept. 30, 2016, using administrative data from the VA and DoD from the Long-term Impact of Military-Relevant Brain Injury Consortium-Chronic Effects of Neurotrauma Consortium. Participants were followed up until Dec. 31, 2018.
Combining data from both health systems allowed the researchers to include a very large cohort of current and former servicemembers with long follow-up times, Stewart explained. Of the 2,530, 875 veterans from the consortium, a total of 1,559,928, were included in the analysis. Participants were predominantly young (younger than 35 at index date) and male.
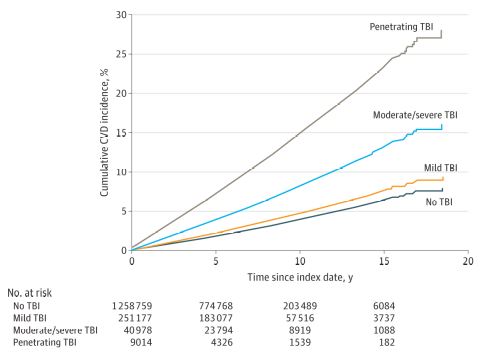
Click to Enlarge: Cumulative Incidence Functions for the Composite Outcome Stratified by Traumatic Brain Injury (TBI) SeverityCVD indicates cardiovascular disease. Source: JAMA Neurology
“We then looked at the impact of an episode of TBI on the subsequent development of cardiovascular disease—which we defined as coronary artery disease, stroke, peripheral artery disease or death from cardiovascular disease,” he advised.
Stewart said the key finding was that veterans with a TBI history were at an increased risk for cardiovascular disease compared to veterans without a TBI history. “There was also the suggestion of a dose-response, whereby more severe TBI resulted in a higher cardiovascular disease risk.”
He emphasized the importance of noting that one source of bias with this type of research is that patients with TBI might seek more care and are thus more likely to be diagnosed with cardiovascular disease. He added, however, that the authors also found that TBI increased cardiovascular death, which was taken from a different data source, the National Death Index. “To me, this implies that the effect we are observing is real and is not due to bias from diagnostic codes,” he said.
“Our study underscores an emerging concept in the field, that TBI is more than an event; it is a disease process. Veterans will continue to have health problems long after their TBI episode,” said Stewart, who cared for more than 250 critically injured patients when he was deployed as an ICU physician to Bagram, Afghanistan.
That is especially significant, because of the sheer number of former military troops affected. The VA reported that more than 450,000 U.S. servicemembers were diagnosed with a TBI from 2000 to 2021.
“The care that our servicemembers received was truly remarkable, as evidenced by our hospital’s 99.5% survival rate,” Stewart said. “However, we cannot define success solely on the basis of short-term outcomes.”
Given the relatively young age of the cohort, these results suggest there may be an increased burden of CVD as these veterans age and develop other CVD risk factors. “The results from our study examines cardiovascular risk and implies that strict control of modifiable risk factors—for example, hypertension—may be important to improve long-term outcomes in veterans with a history of TBI.” Stewart concluded.
- Stewart IJ, Amuan ME, Wang CP, Kennedy E, et. al. Association Between Traumatic Brain Injury and Subsequent Cardiovascular Disease Among Post-9/11-Era Veterans. JAMA Neurol. 2022 Sep 6:e222682. doi: 10.1001/jamaneurol.2022.2682. Epub ahead of print. PMID: 36066882; PMCID: PMC9449870.
