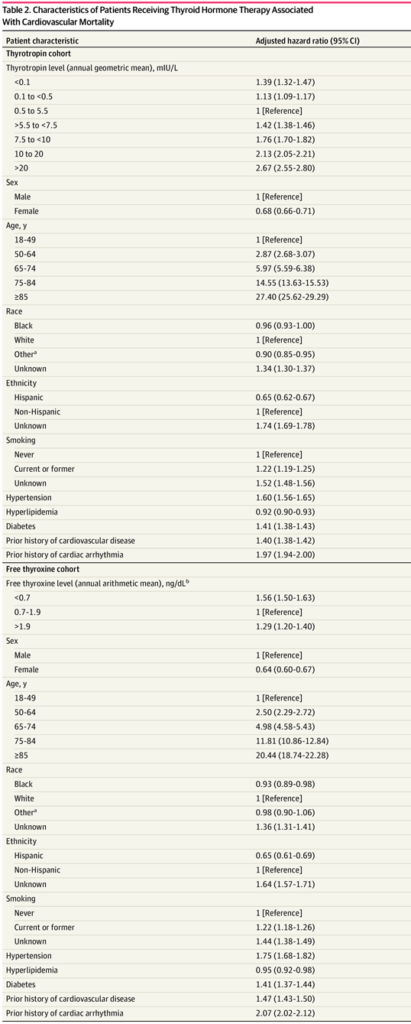
Characteristics of Patients Receiving Thyroid Hormone Therapy Associated With Cardiovascular Mortality.
a. Composed of the following races: Alaska Native or American Indian, Asian, Native Hawaiian or Pacific Islander, and multiracial.
b. To convert free thyroxine to picomoles per liter, multiply by 12.87
Source: JAMA Netw Open. 2022;5(5):e2211863
ANN ARBOR, MI — Both over-treatment and under-treatment with synthetic thyroid hormones are associated with an increased risk of cardiovascular mortality in U.S. veterans, according to a new study.
The retrospective cohort study in JAMA Network Open evaluated the association between the intensity of thyroid hormone treatment and cardiovascular mortality (death from cardiovascular causes, including myocardial infarction, heart failure or stroke). This association has not been previously studied, even though cardiovascular disease is the leading cause of death in the United States, and levothyroxine (the most commonly used synthetic thyroid hormone) has consistently been in the top three most frequently prescribed medications in the U.S. for the past decade.1
The authors analyzed de-identified patient data from the Veterans Health Administration Corporate Data Warehouse database for 705,307 patients aged 18 years or older who received thyroid hormone treatment between Jan. 1, 2004, and Dec. 31, 2017. Those veterans were being treated for hypothyroidism with thyroid hormone. The median patient age was 67 years old, and 625,444 (88.7%) were men.
Of these patients, 701,929 had at least two outpatient measurements of serum thyrotropin between initiation of thyroid hormone treatment and either death or the end of the study. The authors also studied 373,981 patients receiving thyroid hormone treatment who had at least two outpatient free thyroxine (FT4) measurements between initiation of thyroid hormone treatment and death or study conclusion.
Patients with thyroid cancer, missing date of birth and patients on medications known to interfere with thyroid function tests, such as amiodarone and lithium, were excluded. These data were then linked to the National Death Index for mortality ascertainment and to identify cause of death.
Based on the data, 75,963 patients (10.8%) died of cardiovascular causes. The study found over-treatment and under-treatment with thyroid hormone were associated with increased risk of cardiovascular mortality, even when adjusting for demographic factors (such as age, race, sex and ethnicity) and traditional cardiovascular risk factors (such as smoking, high blood pressure, diabetes, previous cardiovascular disease or arrhythmia).
Patients whose thyroid function tests were outside the normal range (exogenous hyperthyroidism and exogenous hypothyroidism) were at higher risk for cardiovascular mortality compared with individuals with euthyroidism (having thyroid function tests within the normal range).
Exogenous hyperthyroidism is defined as giving too much thyroid hormone, leading to thyroid function tests consistent with hyperthyroidism (low TSH, high free T4). Patients with exogenous hyperthyroidism (over-treatment with thyroid hormone) had thyrotropin levels <0.1 mIU/L: adjusted hazard ratio [AHR], 1.39; 95% CI, 1.32-1.47; FT4 levels, >1.9 ng/dL: AHR, 1.29; 95% CI, 1.20-1.40.
Exogenous hypothyroidism means giving too little thyroid hormone, leading to thyroid function tests consistent with hypothyroidism (high TSH, low free T4). Patients with exogenous hypothyroidism (under-treatment with thyroid hormone) had thyrotropin levels >20 mIU/L: AHR, 2.67; 95% CI, 2.55-2.80; FT4 levels, <0.7 ng/dL: AHR, 1.56; 95% CI, 1.50-1.63.
Normal Range
The findings emphasize the importance of maintaining thyroid tests within the normal range to decrease cardiovascular risk and death among patients receiving thyroid hormone treatment. The results suggest the intensity of thyroid hormone treatment may be a modifiable risk factor for cardiovascular mortality.
“Although many cardiovascular risk factors are known, the intensity of thyroid hormone treatment as a modifiable risk factor for cardiovascular risk and its association with cardiovascular mortality was not previously studied,” Maria Papaleontiou, MD, corresponding author and assistant professor in the Division of Metabolism, Endocrinology and Diabetes and research assistant professor in the Institute of Gerontology at the University of Michigan, told U.S. Medicine. “Our prior work using data from U.S. veterans has shown that thyroid hormone use is prevalent in this population, with more than 50% of veterans on thyroid hormone being 65 years and older. Additionally, prior studies in adults with hypothyroidism have shown that up to 30% are under-treated and up to 48% are over-treated; specific to the veteran population, we previously found that almost one-third of U.S. veterans on thyroid hormone are being over-treated.”
Because the VHA population is predominantly male, women are generally underrepresented in studies using the VHA Corporate Data Warehouse database. However, the results of this study are highly clinically relevant because the risk of cardiovascular disease is higher for men and more than 70,000 women were included in this cohort. Also, this was an observational study, and a causal relationship between the intensity of thyroid hormone treatment and cardiovascular mortality could not be definitively established.
To protect the lives of patients, the study’s findings emphasize how important it is for healthcare professionals to actively monitor thyroid hormone treatment.
“In this study, both over- and under-treatment with thyroid hormone were associated with increased cardiovascular mortality when adjusting for a comprehensive set of demographic and traditional cardiovascular risk factors,” Papaleontiou wrote in an email. “Our findings highlight the need for clinicians to make every effort to maintain euthyroidism in patients on thyroid hormone treatment, regardless of underlying cardiovascular risks. This is particularly important in vulnerable populations, such as older adults, who are at higher risk for adverse cardiovascular events with both exogenous hyper- and hypothyroidism. Addressing over- and under-treatment of hypothyroidism will help reduce patient harm.”
- Evron JM, Hummel SL, Reyes-Gastelum D, Haymart MR, Banerjee M, Papaleontiou M. Association of Thyroid Hormone Treatment Intensity With Cardiovascular Mortality Among US Veterans. JAMA Netw Open.2022;5(5):e2211863. doi:10.1001/jamanetworkopen.2022.11863
