Cholesterol-Lowering Treatment Suboptimal in High-Risk Veterans
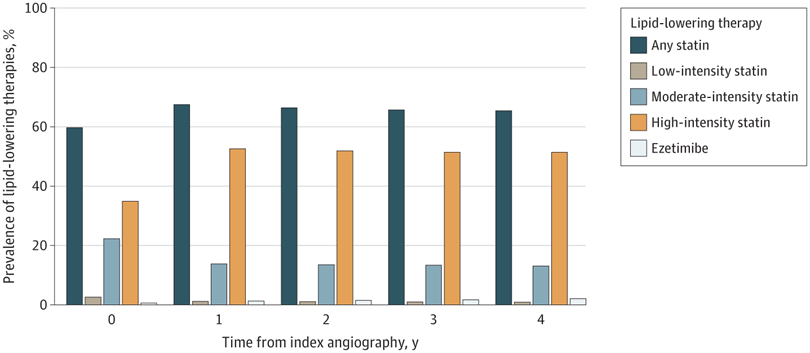
Click to Enlarge: At the time of index coronary angiography, 66 877 patients (59.7%) were prescribed a statin, 39 042 patients (34.9%) were prescribed a high-intensity statin regimen, and ezetimibe use was rare (623 [0.6%]). The proportion of patients prescribed a statin peaked at 3 months following index angiography and then remained generally stable from 6 months through 4 years after index angiography. The use of ezetimibe remained low throughout the study period. Source: JAMA Network Open
The cohort study published in JAMA Network Open examined potential opportunities to reduce adverse cardiovascular events among patients with coronary artery disease using optimized oral lipid-lowering therapy (LLT). The research team included investigators from Rocky Mountain Regional VAMC in Aurora, CO, and the Office of Quality and Patient Safety at VHA in Washington, DC.1
In the study, 111,954 veterans with coronary artery disease were identified by coronary angiography between June 2015 and September 2020 across 82 VA healthcare facilities. The veterans had a mean age of 68.8 years; 97.7% were men, 81.8% were white, 15.7% were Black and 5.3% were Hispanic. The analysis used de-identified patient data from the VA Clinical Assessment Reporting and Tracking (CART) program and administrative data from the VA health record, the study reported.
Patients were followed for up to four years, and the researchers analyzed VA pharmacy, laboratory and clinical data to determine time-varying LLT and corresponding low-density lipoprotein cholesterol (LDL-C) levels and rates of death, myocardial infarction, stroke and coronary revascularization. Observed treatment options were LLT, LLT with an optimized statin regimen and LLT with optimized statin and ezetimibe, the researchers pointed out.
The study noted that “many patients with coronary artery disease don’t achieve the guideline-directed goals for LDL-C levels.” Cholesterol-lowering therapy is “an essential element of secondary prevention for patients with established atherosclerotic cardiovascular disease. For such patients, current U.S. guidelines recommend LLT to achieve an LDL-C level <70 mg/dL and a 50% reduction from untreated levels,” the study authors explained.
“We conducted a study to assess the prevalent use of LLT in patients with proven coronary artery disease in the Veterans Affairs Healthcare System and to gauge the potential for further cardiovascular risk reduction if optimized LLT with statins and ezetimibe were employed,” Christopher Kovach, MD, MSc., an interventional cardiologist and peripheral vascular fellow at Brown University Warren Alpert School of Medicine, told U.S. Medicine.
The research team “projected how much further reduction in LDL cholesterol might have been attained if optimized statin therapy had been utilized, with or without adjunctive use of ezetimibe,” the study authors wrote in an email.
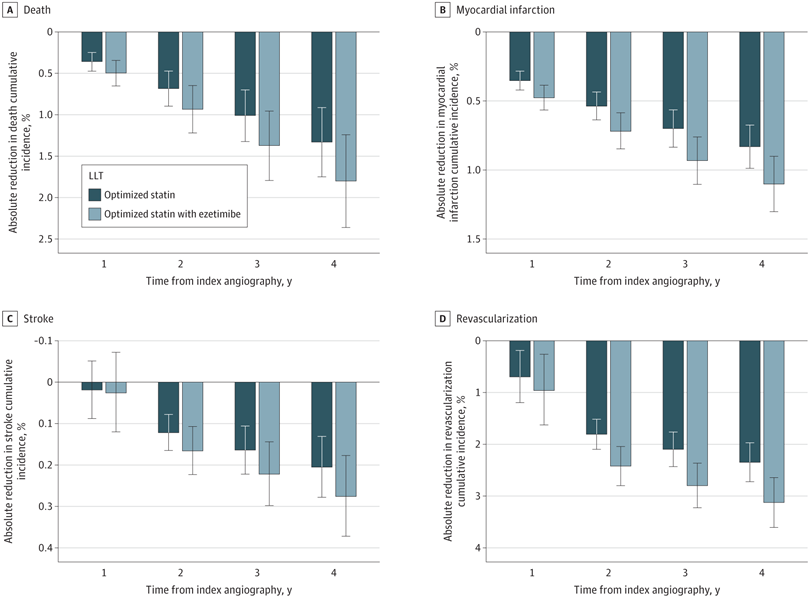
Click to Enlarge: The projected percentage of risk reduction is presented for the cumulative incidences of the following 4 subcategories of adverse events: A, death; B, myocardial infarction; C, stroke; and D, coronary revascularization. The error bars represent 95% CIs. The values were projected for optimized statin therapy alone and for optimized statin therapy with ezetimibe. Source: JAMA Network Open
“Optimized statin therapy was assumed to be atorvastatin 80 mg daily in patients without contraindications,” explained Prerna Gupta, MD, a cardiology fellow at the University of Colorado School of Medicine. “From the potential further reduction in LDL-C with optimized LLT, we projected the potential further reduction in death and cardiovascular events using the formulas developed by the Cholesterol Treatment Trialists’ Collaborative (CTT).”
‘Sizeable Reductions’ in Mortality Risk
The study found that “insufficient LLT was common among veterans with coronary artery disease” and the “widespread use of optimized statin therapy could potentially reap sizeable reductions in the risks of death and cardiovascular events in these patients,” according to the authors.
“Despite the demonstrated efficacy, wide availability, low cost and excellent safety profile of statins and ezetimibe, we found that this veteran cohort frequently received less intensive LLT than recommended by national guidelines,” pointed out Gregory Schwartz, MD, PhD, chief of the cardiology section at Rocky Mountain Regional VAMC in Aurora, CO, and professor of medicine at the University of Colorado School of Medicine. “Specifically, we found that almost a third of patients were not treated with a statin after diagnosis of coronary artery disease, and nearly half were not treated with a high-intensity statin regimen.”
“The mean achieved LDL-C level was approximately 80 mg/dL, and most patients did not achieve an LDL-C goal of <70 mg/dL on prescribed therapy,” Schwartz advised. “The prevalent use of ezetimibe was very low at around 1%. The analysis identified disparities by race, ethnicity and sex in achievement of LDL-C goals, with less frequent achievement in Black and female patients than in white, Hispanic and male patients.”
This veteran cohort “had a high rate of death and cardiovascular events,” the study authors wrote. At 4 years, they observed the following incidences: death (21.6%), myocardial infarction (5.0%), stroke (2.2%) and coronary revascularization (15.4%). They projected that mean achieved LDL-C levels could have been further reduced to approximately 59 mg/dL if statin therapy had been optimized and to approximately 50 mg/dL, had ezetimibe been utilized.
If further reductions in LDL-C had been realized, veteran patients could have experienced an additional decrease in adverse clinical events, which the authors indicated is the most-important finding of the study.
“With optimized high-intensity statin and ezetimibe, we projected absolute reductions from observed levels in the incidence of death, myocardial infarction, stroke and coronary revascularization of 1.8%, 1.1%, 0.3%, and 3.1% at four years,” Kovach said. “Our data indicate a major missed opportunity in secondary prevention of death and cardiovascular events. Our message is that high or maximum indicated intensity statin therapy and adjunctive use of ezetimibe should be employed for all eligible patients to reduce their risk of cardiovascular events, perhaps as a combination pill.”
“There is a window of opportunity at the time of invasive procedural care, when significant healthcare resources are being deployed for an individual patient, to assess current lipid levels and therapies and make appropriate adjustments based on these results,” Kovach advised. “While ezetimibe is less effective than optimized statin, it is well tolerated and could have great benefits on a population level. This is truly ‘low-hanging fruit’ in cardiovascular prevention.”
Newer therapies such as PCSK9 inhibitors “are also powerful tools to lower LDL-C and reduce adverse events. PCSK9 inhibitors weren’t a subject of this analysis, but they’re an important area of future population-level research,” the study authors added.
The findings call for “targeted interventions to promote greater equity in the secondary prevention of cardiovascular disease,” according to the study.
- Kovach CP, Mesenbring EC, Gupta P, et al. Projected Outcomes of Optimized Statin and Ezetimibe Therapy in US Military Veterans with Coronary Artery Disease. JAMA Netw Open. 2023;6(8):e2329066. doi:10.1001/jamanetworkopen.2023.29066

