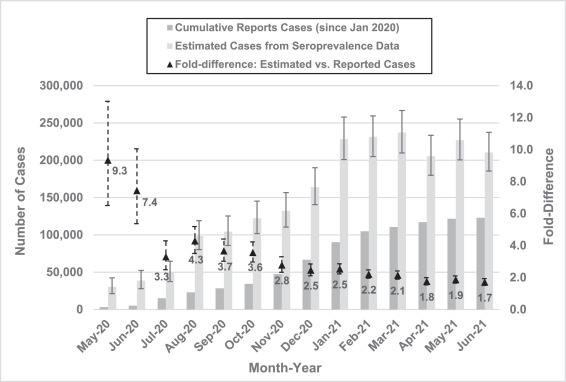
Click to Enlarge: Comparison of seroprevalence estimate of COVID-19 cases with monthly cumulative confirmed cases, May 2020–June 2021. Source: AJPM Focus
BETHESDA, MD — The number of reported COVID-19 cases in active-duty U.S. military members was considerably lower than true cases during the first 18 months of the COVID-19 pandemic, according to a recent study, which used severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) seroprevalence data to reveal the gap.
The longitudinal seroprevalence study published in AJPM Focus “is the largest serologic study of its kind within a well-described population and complements several other cross-sectional seroprevalence studies conducted within civilian populations,” suggested the authors from the Armed Forces Health Surveillance Division of the Defense Health Agency in Silver Spring, MD; Uniformed Services University of the Health Sciences in Bethesda, MD; United States Army Medical Research Institute of Infectious Diseases in Frederick, MD; and the Office of the Assistant Secretary of Defense for Health Affairs in Washington, DC.
For many infectious diseases, “reported confirmed cases represent a small portion of overall true cases, and the undercounting of true cases can be considerable when a significant portion of infected individuals are asymptomatic or minimally symptomatic, such as with COVID-19,” the researchers pointed out. During the first two years of the pandemic, case counts were the primary indicator shared with the public, along with hospitalization rates and death rates, but these measures “provided an incomplete picture of the full scope of the COVID-19 pandemic,” the study team reported in the journal AJPM Focus.1
While molecular testing is “the gold standard for confirming SARS-CoV-2 infection in individuals, serologic surveillance studies provide a unique and efficient means of estimating the full impact of COVID-19,” according to the report. By using the period prevalence of SARS-CoV-2-reactive antibodies across a population, seroprevalence studies are an excellent way to “estimate cumulative case counts because they are able to detect the large number of asymptomatic and minimally symptomatic cases that do not present for molecular testing,” the authors wrote in the paper. During a large-scale outbreak, seroprevalence studies can effectively “assess the extent to which true cases are undercounted and can inform efforts to improve case identification and reporting,” they explained.
The researchers used samples collected from the DOD Serum Repository from 18,581 active duty U.S. military members of all branches collected between May 2020 and June 2021 from locations across the United States. Serum specimens that are left over from routine HIV testing within the U.S. military are submitted to this repository on a regular basis and are available to conduct studies on a range of medical conditions.
A random selection of servicemember serum samples submitted to the DOD Serum Repository “was analyzed for the presence of antibodies reactive to SARS-CoV-2, and the monthly seroprevalence rates were compared with those of cumulative confirmed cases reported during the study period,” the researchers explained.
“We found that the number of true cases of COVID-19 greatly exceeded the number of cases that were being reported through routine surveillance channels,” Kevin M. Taylor, MD, assistant professor and director of the Division of Global Public Health at Uniformed Services University, told U.S. Medicine. “This was much more pronounced in the early months of the COVID-19 pandemic. This did not surprise us, as it was already known that a number of asymptomatic or mildly symptomatic cases were likely unreported. However, this study allowed us to quantify the extent to which this was happening and also understand how this trend changed over time.”
The study found that “seroprevalence was 2.3% in May 2020 and increased to 74.0% by June 2021,” the researchers pointed out. “The estimated true case count based on seroprevalence was 9.3 times greater than monthly reported cases at the beginning of the study period and fell to 1.7 by the end of the study,” the authors reported. The findings show a similar trend in seroprevalence rates in the early phase of the pandemic when compared with data released by the U.S. Centers for Disease Control and Prevention (CDC) from commercial laboratory and blood donor seroprevalence surveys.
The seroprevalence study utilizing the DOD Serum Repository was “a useful and efficient way to assess underestimated true cases of COVID-19, since it did not require us to obtain additional samples from service members above and beyond what was already being obtained as part of routine HIV testing,” Taylor wrote in an email.
While seroprevalence was higher among certain age groups at various points in time during the study, the authors didn’t find any significant difference between these groups over the entire duration of the study, he added.
“We first began exploring SARS-CoV-2 seroprevalence as a means of understanding the overall impact of COVID-19 across the U.S. military, hoping that it would also help us understand the level of immunity that was being achieved over time,” Taylor said. “With the data we obtained, we realized that we could also assess the extent of underreporting of COVID-19 cases that was occurring, and this ended up being an important finding that we felt deserved broader attention.”
“This study really highlights the extent of underreporting that can occur in the face of an epidemic, especially when a significant portion of infections may be asymptomatic or mildly symptomatic,” he added. “This is not a surprising phenomenon, but understanding the extent to which it can occur is important for public health officials to appreciate.”
Healthcare professionals who are trying to assess the full impact (i.e., true number of cases) during an infectious disease epidemic should employ a variety of surveillance modalities, including seroprevalence studies, Taylor recommended. “Each of these modalities has its benefits and shortcomings, but when used in combination can provide a more complete picture of the epidemic, which provides public health officials with the data necessary to make informed decisions.”
“This is not the last time we’ll be faced with the threat of a large-scale epidemic (or pandemic), and it’s important that we appreciate the limitations of routine disease surveillance and case reporting,” he advised. “This study did show that underreporting of cases diminished over time with improved testing capabilities and enhanced efforts at case detection. But it was not eliminated completely, suggesting that seroprevalence studies may be a useful adjunct to routine surveillance well into the course of an epidemic.”
Study authors suggested that “additional cross-sectional seroprevalence studies are needed to continue monitoring these trends because further evolution of SARS-CoV-2 may offer new opportunities for the virus to surge again in populations with diminished immunity.”
- Taylor KM, Ricks KM, Kuehnert PA, Eick-Cost AA, Scheckelhoff MR, Wiesen AR, Clements TL, Hu Z, Zak SE, Olschner SP, Herbert AS, Bazaco SL, Creppage KE, Fan MT, Sanchez JL. Seroprevalence as an Indicator of Undercounting of COVID-19 Cases in a Large Well-Described Cohort. AJPM Focus. 2023 Aug 15;2(4):100141. doi: 10.1016/j.focus.2023.100141. PMID: 37885754; PMCID: PMC10598697.
