WASHINGTON — The VA can learn important lessons from how it handled infection control in its senior centers during the height of the COVID-19 pandemic, according to a recent Government Accountability Office (GAO) report. These lessons could help prepare the department for future waves, as well as other infectious disease emergencies.
According to the report, while VA issued guidance on how to limit infections in its community living centers (CLCs), there was little oversight during peak infection months. This limited how much VA knew about how its CLCs were faring and how things could be improved.
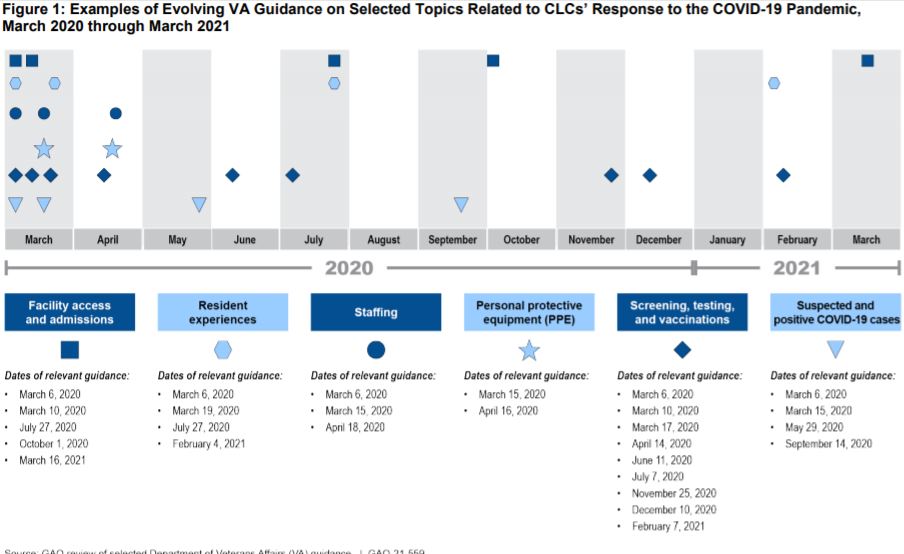
In March 2020, VA shut down its 134 CLCs and spinal cord injury centers to visitors—a move that seemed drastic at the time, when the department was treating only a handful of COVID-positive veterans. As the pandemic worsened, VA began issuing guidance to CLC staff, limiting entry, testing residents and staff for the virus, and training staff for a surge in cases.
VA also suspended annual in-person inspections from March 2020 to February 2021.
“These inspections are VA’s primary means of CLC oversight, which the agency uses to evaluate CLCs on a broad range of quality standards, including those relevant to COVID-19 mitigation,” GAO investigators explained in the report. “VA suspended these inspections, which the agency’s contractor typically conducts in person, because of the risk of contracting or transmitting COVID-19 to CLC residents and staff as well as to inspectors. According to VA officials, they considered conducting virtual inspections early in the pandemic, but the agency first had to modify its contract with the organization that conducts the inspections to allow for this. Once this modification was complete, VA resumed inspections virtually in February 2021.”
Weaknesses in Protocols
In July 2020, with the normal inspections on hold, VA asked its CLCs to complete a one-time self-assessment specific to COVID-19 prevention practices, such as hand hygiene, PPE use and restricting visitors. The self-assessments were designed to help CLCs identify weaknesses in their protocol.
For example, following a self-review, one CLC found that staff were observed not conducting hand hygiene after patient care and that reusable medical equipment was not cleaned between uses. Another CLC reported that the facility was not screening visitors appropriately.
For the most part, CLC managers were left to make improvements on their own, since VA did not finish reviewing the assessments until December 2020—five months after they were completed.
Throughout the lockdown period, VA officials relied on informal communications with CLC staff, mostly in the form of monthly phone calls, to discuss their COVID-19 status and infection prevention practices. During those calls, CLC staff could ask questions and get information about the department’s broader pandemic response efforts.
“Given the informal nature of these calls, they were not designed to allow VA to assess CLC infection prevention and control practices in a standardized and comprehensive manner,” the GAO report stated.
Consequently, for most of the first year of the pandemic, VA did not have a clear picture of where individual CLCs could improve infection control, and CLC managers did not have regular, specific guidance on how to make those improvements.
However, the report is not harshly critical of the results of VA’s efforts. On the whole, VA’s CLCs fared far better than state-run veterans’ homes, with VA officials even being called on to help state homes improve their infection control practices, according to the report. And the gaps in oversight are mostly chalked up to the chaos of pandemic reorganization.
“It is understandable that VA faced challenges that affected its ability to oversee nursing homes during the pandemic, as information about COVID-19 and its mitigation rapidly evolved, and the agency had to respond in real time,” the report’s authors noted.
But moving forward, VA could use its experiences to find ways to close that oversight and inspection gap and provide stronger, clearer communication to CLCs.
“VA could benefit from assessing the decisions and actions related to its oversight of infection prevention and control in CLCs during the first year of the pandemic,” the report concluded. “[They] could better prepare to help CLCs mitigate future infectious disease outbreaks among this vulnerable population.”
According to GAO, VA officials have said they would develop a plan for conducting such an assessment by August 2021.