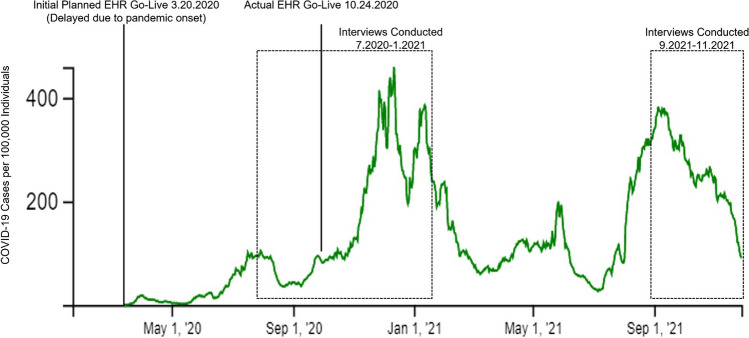
Click to Enlarge: Timeline of an electronic health record (EHR) transition at a Veterans Affairs Medical Center, and the corresponding local trends in COVID-19 cases. Vertical lines and dashed boxes designate key events in the qualitative evaluation of the EHR transition. The green line represents the weekly case rate of COVID-19 per 100,000 individuals in the county where the healthcare facility is located. Source: Journal of General Internal Medicine
BOSTON — Healthcare systems are often required to navigate external stressors, such as policy changes, natural disasters and emerging infectious diseases, which can disrupt patient care. While strategies exist to anticipate and address these challenges, such stressors don’t always occur in isolation. Yet there is little data on how healthcare systems handle multiple organizational stressors simultaneously.
A new study examines how one VAMC fared in late 2020, as it concurrently faced two major disruptions: the anticipated stress of one of the largest electronic health records (EHR) transitions in history—the national conversion from its legacy EHR to Oracle Cerner—and the unexpected stress of a surge in COVID-19 cases. Findings of the study, published in the Journal of General Internal Medicine, demonstrate the importance of healthcare facility preparedness to address the complex interplay of two stressors on employee experience.1
To evaluate the experience of VA clinicians and staff navigating these simultaneous organizational stressors and identify potential strategies to optimize management of co-occurring stressors, researchers led by Justin Rucci, MD, of the Center for Healthcare Organization and Implementation Research at the VA Boston Health Care System analyzed longitudinal qualitative interview data from clinicians, nurses, allied health professionals and local leaders at VA’s initial EHR transition site. The Mann-Grandstaff VAMC in Spokane, WA, was the first facility to undergo the transition.
Interviews were conducted between July 2020 and November 2021—once before and 2 to 4 times after the date on which the health system transitioned. This timing corresponded with local surges of COVID-19 cases.
In general, participants described multiple challenges in navigating the EHR transition and concurrent surges of COVID-19 cases across interview time points. Based on their responses, the researchers identified these five recurring themes describing the simultaneous impact of COVID-19 and EHR transition:
- Efforts to mitigate COVID-19 transmission led to insufficient access to EHR training and support. In response to the challenges posed by the COVID-19 pandemic, the initial VA transition site implemented policies aimed at safeguarding the health and well-being of VA staff. While these strategies—promotion of telework where feasible, the enforcement of masking and physical distancing for in-person employees and the isolation of individuals testing positive for COVID-19—were essential for pandemic management, the authors discovered that they had a detrimental impact on EHR training.
Simultaneously, efforts to curb the transmission of COVID-19 restricted the in-person availability of Cerner staff to provide offer real-time support throughout the EHR transition.
- Clinical practice changes in response to the pandemic impacted EHR workflows in unexpected ways. Participants described how changes to their day-to-day clinical activities driven by the pandemic led to unanticipated challenges working within the new EHR. “For example, unexpected scheduling changes during the pandemic were difficult to monitor and manage in the new EHR system,” the authors wrote.
Other challenges cited by participants included the adaption to different roles because of the pandemic, undergoing an EHR transition while adjusting the expanded telehealth infrastructure, and the reduction in warm handoffs, which decreased the effectiveness of communication among team members and had the potential to limit access to mental health care for patients.
In contrast to these criticisms, some participants did identify a silver lining to the alignment of pandemic surges and the EHR transition. The mandated decrease in patient volume to mitigate COVID-19 transmission allowed more time to navigate the new EHR.
3. Lack of clear communication and inconsistent enforcement of COVID-19 policies intensified pre-existing frustrations with the EHR. “Participants described increasing frustration and conflict within their local teams and the wider VA institution while coping with the pandemic and the EHR transition,” the researchers wrote. “There was a notable desire for improved communication from VA leaders. For example, one participant was dissatisfied with the lack of clarity surrounding the expected volume of in-person patient visits as the number of COVID-19 cases increased.”
The researchers also reported individuals demonstrated differences in commitment to masking, at least partially due to poor communication surrounding masking policy from leadership and lack of effective policy enforcement. “While respondents did not directly describe the interaction between masking and the EHR transition, they noted that variable masking practices negatively affected team dynamics, which could substantially hinder the EHR transition.”
4. Managing concurrent organizational stressors increased work dissatisfaction and feelings of burnout. The overlapping burdens of COVID-19 and the EHR transitions elicited intense emotional responses among many participants. Some described maximal levels of stress among clinicians and staff. Low morale seemed to be a common thread among participants, who noted difficulties keeping a positive outlook in the face of concurrent stressors.
5. Participants had limited bandwidth to manage competing demands that arose from concurrent organizational stressors. There was a pervasive feeling among participants of difficulty managing the demands of multiple simultaneous changes. Participants voiced the belief that the challenges of competing demands could have been avoided by deferring the EHR transition in the face of the obvious burdens of the pandemic.
“The co-occurrence of the COVID-19 pandemic and an EHR-to-EHR transition was profoundly challenging for VA clinicians, nurses, and allied health professionals, who struggled to manage the competing demands of concurrent disruptive events,” the researchers wrote, adding their research offers insight into managing future co-occurring challenges and informing planning and preparation for organizational change. “When possible, healthcare systems should try to anticipate and avoid simultaneous stressors, although it is not always possible to delay necessary organizational initiatives, and unforeseen circumstances may arise.”
They concluded, “future EHR transitions may be less impacted by external stressors if healthcare systems employ flexible implementation strategies within the context of a dynamic sustainability framework, design interventions to mitigate healthcare worker burnout, and optimize communication from leadership.”
- Rucci, J. M., Ball, S., Brunner, J., Moldestad, M., et. al. (2023). “Like One Long Battle:” Employee Perspectives of the Simultaneous Impact of COVID-19 and an Electronic Health Record Transition. Journal of General Internal Medicine, 38(Suppl 4), 1040–1048. https://doi.org/10.1007/s11606-023-08284-3

