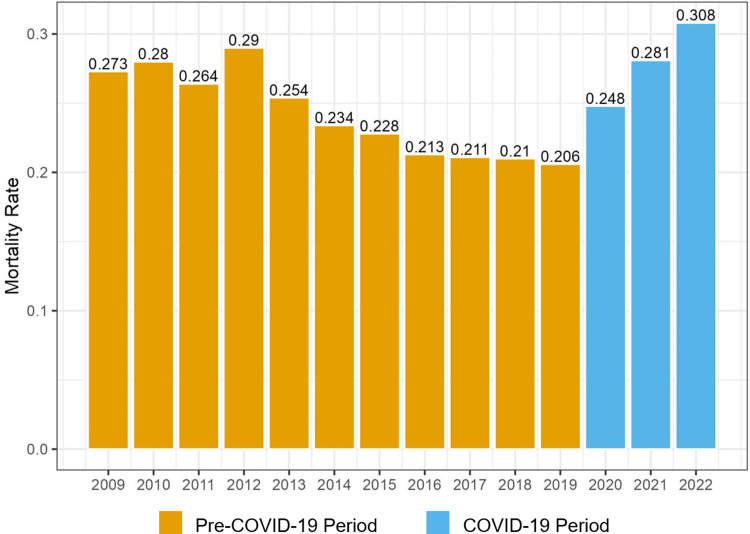
Click to Enlarge: Figure indicates the proportion of PA-BSI cases in the VHA system meeting the primary end point of mortality at 30 d during each year of the study period. Mortality decreased across the pre-COVID-19 period to a low of 20.6% and increased during the COVID-19 period, peaking at 30.8% in 2022 through June 30. PA-BSI, Pseudomonas aeruginosa bloodstream infection; VHA, Veterans Health Administration. Source: Antimicrobial Stewardship & Healthcare Epidemiology
CLEVELAND — Pseudomonas aeruginosa (PA), an opportunistic pathogen commonly associated with healthcare-associated infections, has a high mortality rate. The organism’s high virulence and ability to rapidly acquire resistance to antibiotics make PA infections a treatment challenge.
In 2019, the national Centers for Disease Control and Prevention (CDC) published encouraging data indicating a 30% decrease in multidrug-resistant PA between 2012 and 2017, but in 2020 rates had risen again. In 2022, the CDC reported a 32% increase in rates of multidrug resistant (MDR) PA from 2019 to 2020, largely attributed to antibiotic overuse in patients with COVID-19. In addition to observed higher rates of MDR PA, several studies have identified a recent rise in bloodstream (PA-BSI) incidence, which is especially deadly.
Because Pseudomonas aeruginosa bloodstream infection (PA-BSI) and COVID-19 are independently associated with high mortality, researchers at Case Western Reserve University and Cleveland Clinic sought to understand the impact of COVID-19 coinfection with PA-BSI. Using data from the VHA Corporate Data Warehouse (CDW)—a repository for patient data recorded in the electronic health record for all patients throughout the VHA system—they identified hospitalized patients with PA-BSI in pre-COVID-19 (January 2009 to December 2019) and COVID-19 (January 2020 to June 2022) periods and characterized trends in resistant, treatment over the study period.
Using registry data, the researchers characterized trends in resistance, treatment and mortality over the study period. They used multivariable logistic regression and modified Poisson analyses to determine the association between COVID-19 and mortality among patients with PA-BSI.
A majority of the 6,714 patients with PA-BSI were male, 70 years or older, white and non-Hispanic with multiple chronic comorbid medical conditions, including uncomplicated diabetes mellitus (43.1%), cancer without metastases (42.1%), chronic pulmonary disease (39.8%) and chronic renal disease (34.2%).
Throughout the study period, PA resistance rates decreased. Overall, 30-day all-cause mortality decreased among case patients during the pre-COVID-19 period, the researchers reported in Antimicrobial Stewardship & Healthcare Epidemiology. Conversely, they observed an increase in 30-day mortality among all case-patients during the COVID-19 period (not stratified by COVID-19 coinfection status).
Case-patients identified in either period were similar in terms of age, comorbidities and severity of illness. Case-patients with COVID-19 coinfection in the COVID-19 period had a 30-day mortality rate of 47.2%, whereas case-patients without COVID-19 during the COVID-19 period and case-patients in the pre-COVID-19 period had similar, lower mortality rates of approximately 25%. In addition to COVID-19 coinfection, predictors of higher mortality included a higher Charlson Comorbidity Index, greater disease severity as measured by the modified Acute Physiology and Chronic Health Evaluation (mAPACHE) score and no targeted PA-BSI treatment within 48 hours.
“While the mortality rate among case-patients increased during the COVID-19 period compared to the pre-COVID-19 period, the COVID-19 period itself did not appear to be associated with increased mortality independent of COVID-19 coinfection,” the authors wrote. “This remained true even when isolating the late-pre-COVID-19 period, corresponding to the 3 years immediately preceding the COVID-19 period with the lowest observed mortality rate of the entire study period. These results suggest that COVID-19 coinfection may account for the increased PA-BSI mortality observed during the COVID-19 period.”
The authors said several factors could account for the increased mortality among patients coinfected with BSI and COVID-19. For example, excessive focus on the diagnosis of COVID-19 infection might delay recognition and workup of coexisting or secondary processes, thereby delaying initiation of appropriate treatment. Logistical barriers could affect management and subsequent outcomes in patients with COVID-19, related to isolation procedures and the need for personal protective equipment. Additionally, circumstances at the institutional level related to the pandemic period, such as nursing- or provider-to-patient ratio, hospital volume and availability of infectious diseases’ expertise could impact outcomes on an individual level. Finally, the interaction of the two infectious processes could lead to a synergistic or additive effect on infectivity and the host response.
‘Rich Database’
The new study, the first to examine the impact of the COVID-19 pandemic on outcomes for patients with PA-BSI, was possible because of the VHA CDW, which “serves as a rich database for this study, capturing data from over 150 medical centers throughout the continental United States and Puerto Rico and spanning a period of almost 20 years,” they wrote. Moreover, the VHA data regarding resistance trends generally align with CDC data in that rates of MDR PA infection were observed to decrease in the last decade until 2020 when an increase was observed.
The authors said their findings laid the groundwork for many potential future studies. “The relationship between COVID-19 and PA should be explored in more detail to determine whether characteristics of either pathogen enhance the infectivity of the other or work synergistically against the host immune response, and inclusion of observations of patients with COVID-19 with and without PA-BSI could be helpful to this end,” they wrote. “More features related to the COVID-19 period would also be worthwhile to investigate, such as impact of staffing, hospital volume, and resources on PA-BSI-associated outcomes.”
- Hojat LS, Wilson BM, Perez F, Mojica MF, Singer ME, Bonomo RA, Epstein LH. Association of COVID-19 coinfection with increased mortality among patients with Pseudomonas aeruginosa bloodstream infection in the Veterans Health Administration system. Antimicrob Steward Healthc Epidemiol. 2023 Dec 15;3(1):e237. doi: 10.1017/ash.2023.455. PMID: 38156202; PMCID: PMC10753479.
