Two-Year All-Cause Mortality Increased, However
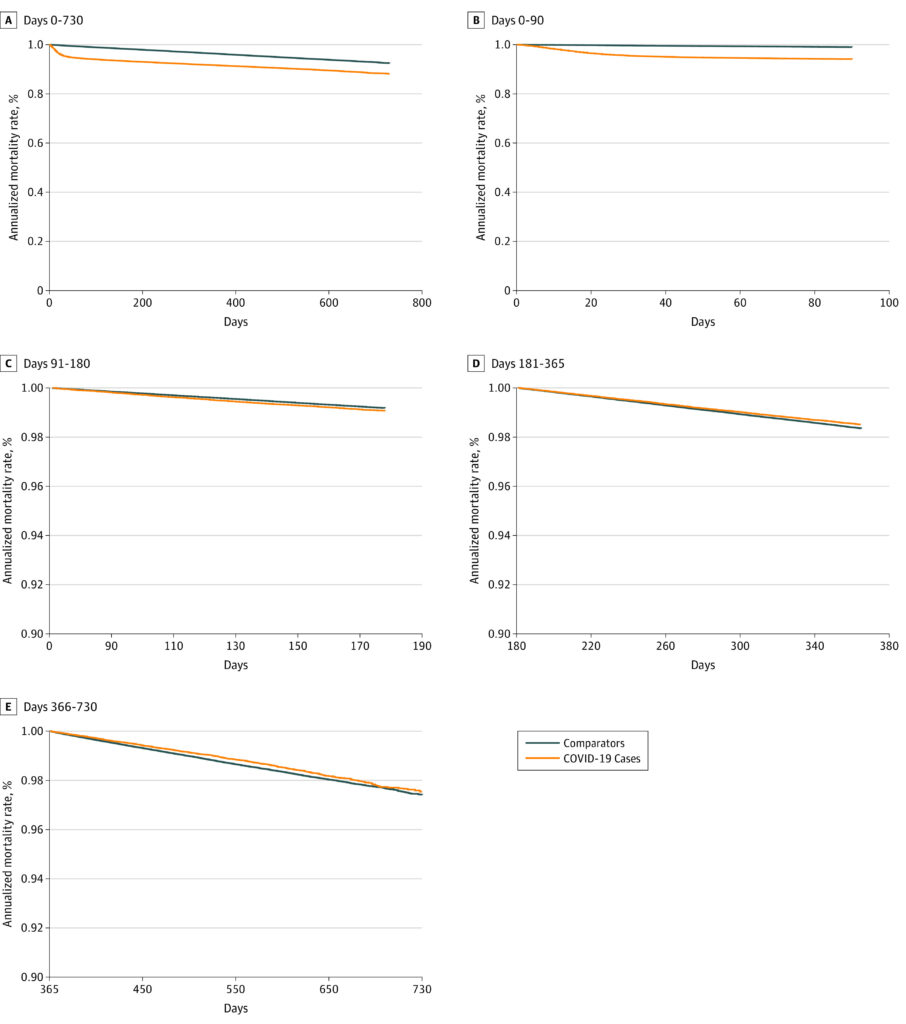
Click to Enlarge: Overall and Time Since Infection-Specific Mortality, From With Censoring, Unweighted Approach
Figure panels C, D, and E have different y-axis scaling to allow for clearer interpretation. Source: JAMA Internal Medicine
ANN ARBOR, MI — The devastating toll of acute COVID-19 infections on human lives is well documented. Yet a pressing question remains: Do survivors of acute COVID-19 face a higher risk of mortality in the aftermath of their infection and, if so, for how long does this risk persist?
In a new study led by Theodore J. Iwashyna, MD, PhD, researchers sought answers in VA electronic health records by examining the mortality of patterns of veterans who had their first documented COVID-19 infection between March 2020, with follow-up data available until April 2022. The study focused on two key periods: acute mortality (within 90 days of infection) and later mortality (days 181-365 and days 366-730).
Iwashyna, a critical care physician and health services researcher at the University of Michigan’s and the Ann Arbor, MI, VAMC’s Critical Care Medicine units, and his colleagues compared the death rates of 208,061 COVID-19 survivors with 1,037,423 matched uninfected comparators with similar characteristics who were alive and uncensored at the beginning of each period. They employed trial emulation methods—comparison of a target trial vs. the authors’ observational emulation—to ensure robust comparisons and also performed a post-hoc analysis of mortality risk by subgroups to understand whether COVID-19 disproportionately increased mortality for those who were already most likely to die.1
The study found that overall 2-year mortality rate was greater among those who had survived COVID-19 than among the uninfected matched comparators. No evidence of excess late mortality relative to risk-matched uninfected comparators was identified, however, the authors reported in JAMA Internal Medicine.
“In fact, there was evidence of reduced mortality among veterans who survived COVID-19 by at least 180 days, which was robust to multiple sensitivity analyses and subgroup analyses,” the researchers wrote. “This finding did not appear to be explained by observed later infections among comparators or elevated mortality not attributable to COVID-19 among high-risk groups.”
The authors said they did not see evidence of consistent excess mortality at the population-level or in those not initially hospitalized for COVID-19, as might have been expected given the concerns regarding incident highly morbid new diagnoses among COVID-19 survivors.
Willingness to Seek Care.
They noted that multiple credible mechanisms responsible for their finding that should be evaluated. “For example, it is possible that the substantial attention to COVID-19 and its sequelae produced relatively greater access to and/or greater willingness to seek care for COVID-19 survivors, and that this greater attention to their medical needs has been beneficial,” they wrote. “Our data cannot distinguish benefits of better access to care among patients with COVID-19 from adverse effects of care disrupted or missed by comparators.”
It is also is possible that these COVID-19 infections conveyed resistance to future severe infections, or there were immunologic or other priming mechanisms from the wide-ranging physiologic changes described after COVID-19, the authors noted.
They stressed these data, only two years into the pandemic, are not the final word and that ongoing follow-up will be essential.
“These results may suggest that, for ongoing care after COVID-19, especially among those not initially hospitalized for COVID-19, efforts that focus on increasing survival may be less relevant than approaches addressing the needs of individual survivors,” according to the study. “These results also have implications for studies of the sequelae of COVID-19, in which differences in mortality, and thus, differential time at risk must be considered.”
The bottom line: Understanding the time course of excess mortality after COVID-19 is crucial for healthcare professionals caring for survivors, particularly those dealing with post-COVID-19 conditions. Moreover, this knowledge informs health system planning, helping allocate resources effectively to address the long-term needs of COVID-19 survivors.
- Iwashyna TJ, Seelye S, Berkowitz TS, Pura J, VA HSR&D COVID-19 Observational Research Collaboratory, et. al. . Late Mortality After COVID-19 Infection Among US Veterans vs Risk-Matched Comparators: A 2-Year Cohort Analysis. JAMA Intern Med. 2023 Aug 21:e233587. doi: 10.1001/jamainternmed.2023.3587. Epub ahead of print. PMID: 37603339; PMCID: PMC10442778.

