DANVILLE, IL — From almost the very start of the pandemic, nursing homes and long-term care facilities proved to be particularly vulnerable to the virus. The close quarters combined with elderly patients suffering from preexisting illnesses resulted in a number of outbreaks and a much higher death rate than the general population.
Throughout most of the pandemic, VA has been able to boast that their VA-run community living centers (CLCs) escaped the tragic outbreaks seen in many private and state-run veterans homes. VA officials credited their success to the larger number of medical personnel, the fact that most CLCs are attached to medical facilities and their rigorous infection control procedures.
In October and November 2020, however, an outbreak at a CLC at the VA Illiana Health Care System, which services central Illinois and western portions of Indiana, demonstrated what happens when VA’s infection control fails. That fall, 11 residents died and 239 patients and 92 staff members were diagnosed with COVID-19.
A VA Office of the Inspector General (OIG) report released last month details extensive mismanagement by CLC administrators and a failure to comply with the infection control procedures that had protected most of VA’s other long-term care facilities.
When the pandemic emerged in January 2020, VAMCs across the country developed complex action plans to prepare for a surge in COVID cases. This included the VA Illiana Health Care System, which created a pandemic action plan with 46 items accounting for staff and visitor screening, COVID-19 staff education, PPE inventory and other details. The facility director held regular virtual town hall meetings to update staff on the pandemic.
During the early months, the region and the facility were only lightly touched by the virus, and by June the facility’s pandemic “command center” was stood down.
Beginning in August, the number of new COVID-19 cases in Vermillion County, where the facility is located, began to rise, as did the number of staff and patient cases at the facility as a whole. But it wasn’t until October that the CLC outbreak began, and it happened swiftly.
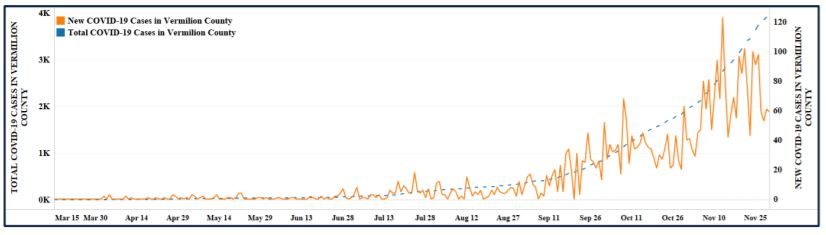
Click to Enlarge: The number of new and total number of COVID-19 cases in Vermilion County, Illinois, from March 15, 2020, through November 30, 2020.
Source: The data represented in this chart are sourced from Johns Hopkins University’s Center for Systems Science
and Engineering
The Danville CLC, which provides rehabilitation, dementia and Alzheimer’s care, geri-psychiatric care, palliative care and extended care services, is split into four “neighborhoods.” On Oct. 13 and 14, the residents of the Victory and Unity neighborhoods all tested negative for COVID-19. On Oct. 17, one staff member of Victory tested positive. On Oct. 18, two additional staff members and two residents of Victory tested positive. On Oct. 19, four staff members of Unity tested positive. On Oct. 20, two residents of Unity tested positive.
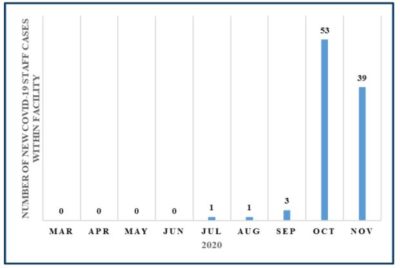
Click to Enlarge: The number of new COVID-19 staff cases from March 15, 2020, to November 30, 2020.
Source: Department of Veterans Affairs COVID-19 National Surveillance Tool: COVID-19
National Summary.
The outbreak would continue through Nov. 17, ending only when the last infected patient died from the virus.
According to the OIG report, while the facility had focused on a potential COVID-19 surge from veterans who live in the region and from nonveterans community members that the facility might be called on to support, it neglected creating a plan for an upsurge within its own CLC.
It was not until after the outbreak occurred that the facility developed a CLC upsurge plan and an outbreak isolation protocol. Infected and noninfected patients were allowed to comingle before the facility opened an unused unit for COVID-19 patients on Oct. 21.
“The OIG found the facility did not have a comprehensive plan that specified operational details such as roles, actions, and targeted time frames for transfer and isolation of CLC residents suspected of, or diagnosed with, COVID-19,” the OIG report states. “The lack of a plan was likely a contributory factor for two COVID-19 positive residents remaining at the CLC for 20 hours after a CLC physician was notified of the positive diagnoses.”
The CLC were also lax in isolating staff members who reported symptoms. When one staff member reported experiencing COVID-19 symptoms, they were instructed to wear a mask and to continue serving CLC residents. The employee later tested positive.
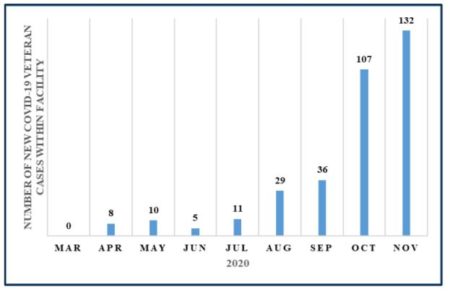
Click to Enlarge: The number of new COVID-19 veteran cases within the facility, both inpatient and outpatient, from March 15, 2020, through November 30, 2020.
Source: VA COVID-19 National Surveillance Tool: COVID-19 National Summary.
CLC employees were left out of the facility’s respiratory protection program and were not all fitted and issued N-95 masks.
Investigators also discovered that the CLC neglected to cancel group activities. CLC residents attended group therapy sessions during the outbreak. While the facilitator wore a mask during the sessions, the residents did not. Two of the Unity residents who tested positive did so the day after attending group therapy sessions. Three of the Victory residents tested positive after attending sessions three days earlier with six other residents.
Once the outbreak was underway, the facility lacked a plan for post-baseline testing with no formalized process for the weekly tracking of COVID-19 testing of staff and residents.
“The failure to test represents a missed opportunity to promptly identify and isolate residents and staff diagnosed with COVID-19 to reduce further transmission of the virus and may have led to staff members working while having COVID-19,” the report states.
The report includes a number of recommendations, including that VA evaluate the incident to determine whether administrative action is warranted. During their investigation, the OIG could find no evidence that any punitive action had been taken by facility leaders.
In a response to the report, Acting Medical Center Director Staci Wiliams, PharmD, RPh, said, “The cases in our Community Living Center impacted our entire staff and reinforced our commitment to learning and improving from the experience. As healthcare professionals, we find it difficult to accept the loss, especially as our staff were heavily invested in providing quality care and maintaining patient and staff safety throughout this pandemic.”
- VETERANS HEALTH ADMINISTRATION, Failure to Mitigate Risk of and Manage a COVID-19 Outbreak at a Community Living Center at VA Illiana Health Care System in Danville, Illinois. VA OIG: #21-00553-285
