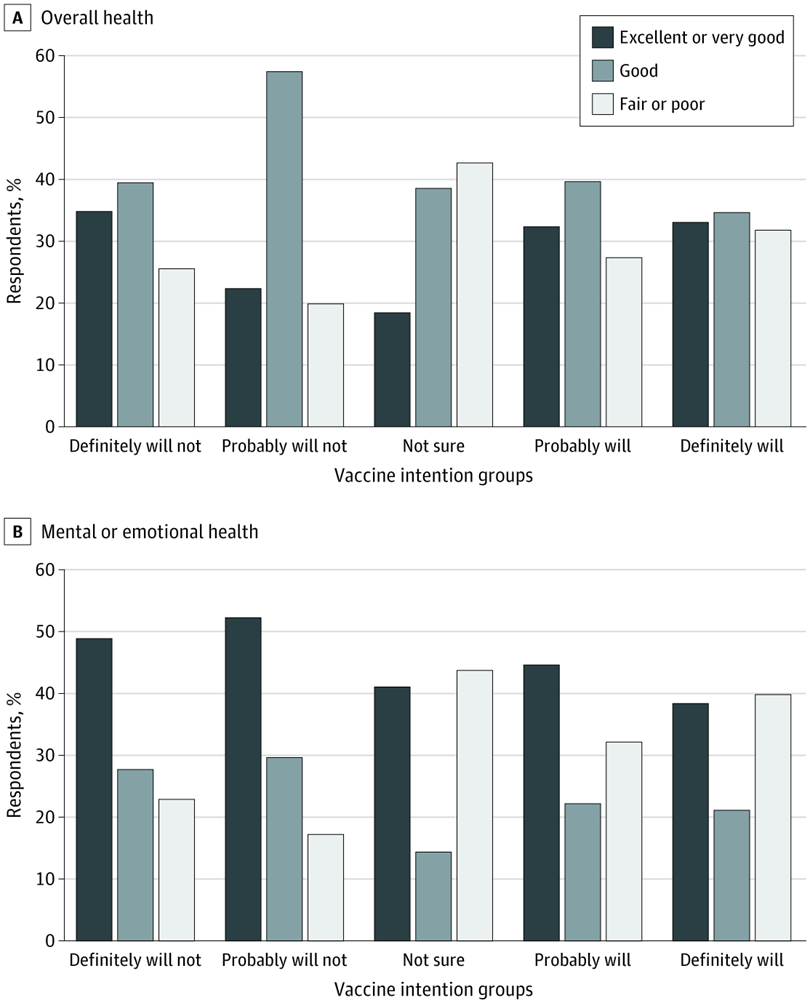
Click to Enlarge: Overall Health and Mental or Emotional Health by Vaccine Intention Groups Among Veterans Who Have Not Yet Been Vaccinated
BEDFORD, MA — Early in 2021, more than one-fourth of veterans responding to a survey said they were concerned about getting a COVID-19 vaccine. The VA has worked steadily since then to change their minds.
In the study regarding U.S. veterans’ attitudes and intentions associated with the COVID-19 vaccination, 29% of veterans surveyed reported not getting the vaccine due to fears about side effects and worry about the newness of the vaccines as primary reasons for not getting vaccinated.
The study survey, published in November in JAMA Network Open, showed that, of 1,178 U.S. veterans who participated in the survey, 71% reported being vaccinated against COVID-19. The cross-sectional, web-based survey study utilized data from the Va Survey of Healthcare Experiences of Patients’ Veterans Insight Panel, fielded in March of 2021.
Some 3,420 veterans were sent a link to complete a 58-item web-based survey, and 34% completed the survey. The data was analyzed from April 1 to Aug. 25, 2021.
“Veterans are a group who experience greater disease burden from COVID-19,” the introduction to the survey results stated. “As trust in government is an important factor associated with vaccine acceptance, vaccine hesitancy in veterans receiving care in the VHA, who are former soldiers and direct recipients of government care, requires examination, considering veterans have a complex relationship with the government compared with the general population.”
As of Dec.19 2021, there had been more than 17,000 known COVID-related deaths among veterans receiving care in the VHA and 805,000 total deaths in the United States attributed to COVID-19.
Also, there are continued variants that have developed, one of the most recent the omicron variant, which has overcome the delta variant as the most common in the United States.
One of the study authors, Guneet Jasuja, PhD, MPH, health research investigator at Edith Nourse Rogers Memorial Veterans Hospital, part of the VA Bedford, MA, Healthcare System, was asked by U.S. Medicine if she was surprised that even more U.S. veterans who responded to the survey had not gotten the vaccine yet, and she said not necessarily.
“The survey was conducted at a time when not everyone in the U.S. who wanted a vaccine was able to get one, due to eligibility reasons, or for other logistical reasons, such as getting time off work or having transportation,” Jasuja responded. “This was true for veterans, as well. But the Veterans Health Administration did enormous outreach through mobile traveling vaccine units to reach Veterans who would find it really difficult to get vaccinated at a medical center or community-based outpatient clinic, such as Veterans living in rural parts of the country. Knowing that some reasons for not yet getting vaccinated were not due to hesitancy but due to logistical reasons really drove these innovative efforts to increase veterans’ vaccinations.”
Jasuja also is an assistant professor at the Boston University School of Medicine.
Also, among those survey respondents who were not vaccinated, those unsure of getting vaccinated were more likely to report fair or poor overall health and mental health than other nonvaccinated groups, the authors pointed out.
Among the 29% of respondents who were unvaccinated, 40% of that group reported they would probably not or definitely would not get vaccinated.
Trusted VA Practitioners
The findings suggest that “targeting veterans’ concerns around the adverse effects and safety of COVID-19 vaccines through conversations with trusted VHA health care practitioners is key to increasing vaccine acceptance,” according to the study.
Out of the 339 survey participants who were not vaccinated: 120 respondents were concerned about side effects; 65 preferred using few medications; 63 preferred gaining natural immunity; 74 preferred to wait because the vaccine is new; and 61 did not trust the health care system.
Of veterans who were not yet vaccinated but who reported that they “definitely will,” 58% agreed both that receiving the vaccination “will contribute to ending the COVID-19 pandemic,” and “it is the best way to prevent others from getting COVID-19.” Those were the two top most-motivating reasons for getting the COVID-19 vaccination. The next top reason (55%) was, “it is the best way to prevent me from getting sick from COVID-19.”
Among respondents who were vaccinated, 57% said that preventing oneself from getting sick was a top reason for getting vaccinated, while 56% said contributing to the end of the COVID-19 pandemic was their main reason.
“As an embedded quality improvement team within the VHA system, our task was to rapidly yet rigorously evaluate the implementation of COVID-19 vaccines,” the survey authors said. “Thus, the goal of this study was to assess veterans’ attitudes and intentions regarding COVID-19 vaccination in the specific context of the VHA system to inform ongoing, systemwide communication efforts to increase the uptake of the vaccines.”
Among the more than 1,100 respondents, 83% were men, 11% were women and less than 1% were transgender or nonbinary. Also, 84% were non-Hispanic white, 5% were Black, and just under 5% were Hispanic or Latino. The mean age of respondents was 66.7 years.
The proportion of respondents trusting their VA healthcare practitioner as a source of vaccine information was higher among those unsure about vaccination compared with those who indicated they would definitely not or probably not get vaccinated 26% vs. 15%, according to the report.
“Implementation of study findings into practice, including patient-provider conversations around vaccine hesitancy, specifically vaccine skepticism, deliberation and distrust has already been underway,” Jasuja advised. “Working with the National Center for Health Promotion and Disease Prevention (NCP), the VHA program office leading vaccine distribution across the VA and drawing on qualitative data collected from 31 veterans and 32 VA employees in another project (Elwy et al., 2021; https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8457639/), our team created a ‘3-Step Plan for Reaching Vaccine Acceptance’, which has been disseminated widely across the VA healthcare system. This plan involves patient-centered communication strategies delivered by trusted healthcare providers and focuses on addressing expected benefits for family, friends and society from the receipt of COVID-19 vaccine.
“More importantly, as suggested by senior author, Dr. Rani Elwy in a previous interview (with U.S. News & World Report), ‘One conversation is never going to be enough to have a shared understanding of this problem of vaccine hesitancy. Hopefully, through continued conversations over time with trusted providers, vaccine hesitancy can move to vaccine acceptance.’”
- Jasuja GK, Meterko M, Bradshaw LD, et al. Attitudes and Intentions of US Veterans Regarding COVID-19 Vaccination. JAMA Netw Open. 2021;4(11):e2132548. doi:10.1001/jamanetworkopen.2021.32548

