WEST HAVEN, CT — Most U.S. veterans who own firearms believe that clinicians should discuss firearm safety, if the patient or the patient’s family members are at increased risk of firearm injury, according to a recent study.
The cross-sectional study published in JAMA Network Open assessed whether U.S. veteran firearm owners believe that firearm safety counseling should occur in clinical settings when patients or their family members are at heightened risk of firearm injury. The study included researchers from the VA Connecticut Health Care System in West Haven.1
For the past two decades, the suicide rate among U.S. veterans has been higher than among nonveterans matched for age and sex, partly because of higher rates of firearm suicide. In 2019, the VA and DoD updated their Clinical Practice Guidelines for the Assessment and Management of Patients at Risk for Suicide in response to elevated veteran suicide rates.
These guidelines recommended that “clinicians assess firearm access as part of a broader strategy to identify suicide risk factors and discuss ways to reduce firearm access with veterans identified as at heightened risk.” The effectiveness of these recommendations is not yet known, and their success depends on clinicians being willing to discuss firearm-related risk with veterans who own firearms, which is about 50%.
Studies have found these discussions initiated by clinicians are uncommon, even among patients receiving care for mental health conditions, partly because of the perception that firearm owners may be opposed to discussing firearms, the study reported.
The current study is the “first nationally representative survey to assess the extent to which veteran firearm owners endorse firearm safety counseling in clinical settings when a patient or a patient’s family member is at risk of firearm injury,” according to the study.
The study analyzed data from the 2019 National Firearms Survey, a nationally representative survey of Americans who resided in households with firearms. Among the 4,030 adults living in households with firearms who completed the survey, 678 adults (mean age 64.7 years old) identified as veteran firearm owners.
Of these veteran firearm owners, 638 were male, most were 60 years or older, 36.5% had served in combat, 80.5% separated from the military before 2002, and 31.5% reported they had used VHA healthcare services in the previous 12 months. They were 9.3% Hispanic, 10.1% non-Hispanic Black, 75.1% non-Hispanic white and 5.5% non-Hispanic other (American Indian or Alaska Native, Asian, Native Hawaiian or Pacific Islander, or more than one race), the study reported.
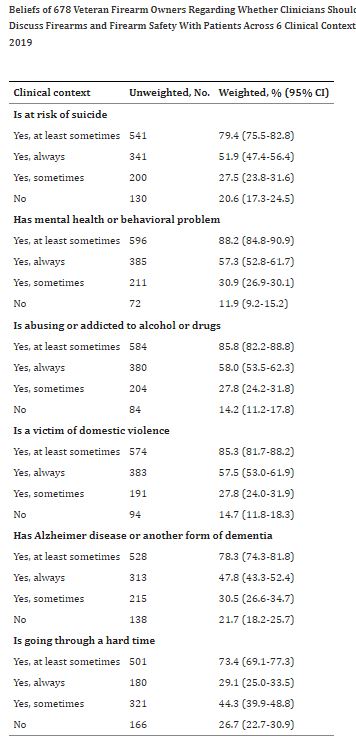
Participants were asked, “As part of routine care, should physicians and/or other health care professionals talk with their patients about firearms and firearm safety if their patient or their patient’s family member (is at risk of suicide; has mental health or behavioral problems; is abusing or addicted to alcohol or drugs; is a victim of domestic violence; has Alzheimer’s disease or another dementia; or is going through a hard time)?” The response options included “No,” “Yes, sometimes,” and “Yes, always.” Responses were divided as “Yes, at least sometimes” and “No,” according to the study.
‘At Least Sometimes’
“We found that most veteran firearm owners believed that clinicians should ‘at least sometimes’ discuss firearm safety across all assessed clinical contexts: elevated suicide risk, mental health or behavioral problems, drug or alcohol problems, domestic violence, having a hard time and dementia,” Frances Aunon, PhD, research psychologist at West Haven, CT, VA Connecticut Healthcare System and associate research scientist at Yale School of Medicine, told U.S. Medicine.
Across the six clinical contexts, support for clinicians “at least sometimes” discussing firearm safety as part of routine care ranged from 73.4% when someone is “going through a hard time” to 88.2% when someone has “mental health or behavioral problems.” When a patient or family member is at risk for suicide, 79.4% of veteran firearm owners responded that clinicians should “at least sometimes” discuss firearms and firearm safety,” the study reported.
The researchers found that “veterans who reported having used VHA services within the prior year were at least as likely to endorse firearm safety conversations compared to veterans who had not used VHA services,” Aunon wrote in an email.
“We also found few regional differences in veterans’ perspectives: at least two-thirds of veterans endorsed firearm safety conversations ‘at least sometimes’ regardless of where the veterans lived,” she said.
The findings suggest that “discussing firearms and firearm safety in clinically indicated situations is viewed as an acceptable routine practice by most veteran firearm owners,” Aunon explained, adding, “We hope these findings help allay clinician concerns about discussing firearm access with veterans with heightened risk of suicide and other firearm injuries. We recommend that healthcare professionals initiate evidence-based discussions regarding firearm injury prevention with veterans when those discussions are clinically indicated.”
Most efforts to prevent firearm injuries among adults in clinical spaces have focused on suicide, but assault-related and unintentional firearm injuries also are important causes of morbidity and mortality among the U.S. population, including veterans. Because the survey questions weren’t specific to suicide and assessed scenarios that place people in the home at heightened risk of firearm assault and unintentional firearm injury, the study’s findings “provide support for clinic-based initiatives aiming to prevent injuries from other intents or within other clinical scenarios, such as in dementia care or within the context of intimate partner violence,” the study reported.
Limitations of the study include that data are self-reported (including veteran status) and that misclassification is possible. Also, social desirability or selection biases could have skewed findings, according to the study.
The study “doesn’t explain why some respondents report that clinicians should never ask about firearms in the clinical contexts that were examined (12% to 27%, depending on the scenario), so further work is needed to better understand the perspectives of these individuals.” It also doesn’t “assess how prior experience discussing firearms with clinicians may influence whether these conversations are seen as an acceptable part of routine care,” the study explained.
- Aunon FM, Azrael D, Simonetti JA, Miller M. Beliefs Among Veteran Firearm Owners Regarding Whether Clinicians Should Discuss Firearm Safety With Patients. JAMA Netw Open. 2023 Jun 1;6(6):e2321219. doi: 10.1001/jamanetworkopen.2023.21219. PMID: 37382951; PMCID: PMC10311384.