Researchers Said They Found ‘Unexpected’ Result
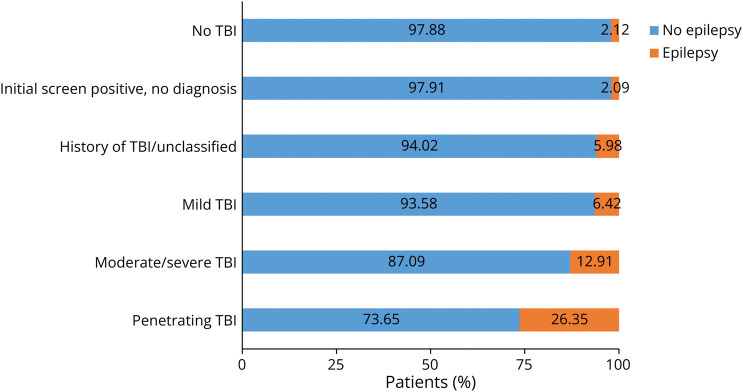
Click to Enlarge: Percentage of Epilepsy by TBI Status (N = 938,890) Blue bars (nonepilepsy) and orange bars (epilepsy) sum to 100%. TBI = traumatic brain injury. Source: American Academy of Neurology
SALT LAKE CITY — Deployment history appears to play a role in the association between traumatic brain injury (TBI) and epilepsy in recent veterans—but not always in an obvious way.
A study in the journal Neurology noted that TBI is a well-established epilepsy risk factor and is common among servicemembers. It added that deployment-related TBI, where combat/blast may be more common, might have different outcomes than nondeployment-related TBI.1
The study led by the VA Salt Lake City Health Care System examined associations of all TBI exposures—not limited to combat—and epilepsy: The researchers adjusted for comorbidities associated with epilepsy, among veterans by deployment status.
Included in the cohort were 938,890 post-9/11 veterans with two or more years of care in both the VHA and DHA systems. Epilepsy was identified through ICD-9/10-CM codes, anti-seizure medication and service-connected disability for epilepsy. Of the cohort, 27,436 (2.92%) had epilepsy. Most veterans had a history of deployment (70.64%).
“Traumatic brain injury is a common effect of post-9/11 deployments due to accidents and explosions (e.g., roadside bombs, improvised explosive devices),” Mary Jo Pugh, PhD, a research career scientist at VA Salt Lake City Health Care System, told U.S. Medicine. “Much of what we know about traumatic brain injury outcomes in post-9/11 era veterans is associated with deployment. However, most traumatic brain injuries that occur in service members occur in a garrison or non-deployed setting.”
The South Texas Veterans Health Care System in San Antonio; the VA Connecticut Health Care System in West Haven; the Uniformed Services University of the Health Sciences in Bethesda, MD; the Central Virginia VA Hospital in Richmond; the Providence, RI, VAMC; and the VA Pittsburgh.
The study authors “hypothesized that, when all traumatic brain injuries are examined, individuals with a deployment-related traumatic brain injury would be more likely to have subsequent epilepsy than those who experience traumatic brain injury in a non-deployed setting,” Pugh explained. However, they didn’t arrive at the expected results, according to the study.
“Overall, we found a much-higher prevalence of epilepsy in our cohort than would be expected in a civilian population of a similar age (~2.9% vs. ~1%), and that veterans who were not deployed (~31% of the cohort) were more likely to experience epilepsy than those who were deployed (~3.9% vs. 2.5%). This occurred despite the fact that deployed veterans were significantly more likely to experience traumatic brain injury,” Pugh said.
The study pointed out that deployed veterans were more likely to have had TBI, compared with the nondeployed veterans (33.94% vs. 14.24%), but nondeployed veterans with moderate/severe TBI had higher odds of epilepsy compared with deployed veterans (adjusted odds ratio [aOR] 2.92, 95% CI 2.68-3.17 vs aOR 2.01, 95% CI 1.91-2.11).
Penetrating TBI
In addition, those with that penetrating TBI had higher odds of epilepsy among the deployed veterans (aOR 5.33, 95% CI 4.89-5.81), but the odds of epilepsy for mild TBI did not significantly differ by deployment status.
The study concluded that deployment history had a “significant differential impact on epilepsy predictors.”
The research team also examined the impact of other epilepsy risk factors (e.g., brain tumor, depression/bipolar disorder and dementia) by deployment status.
The researchers added, “As expected, penetrating TBI had a greater epilepsy impact among deployed veterans perhaps due to combat/blast. Some epilepsy predictors (moderate/severe TBI, multiple sclerosis and Parkinson’s disease) had a stronger association in the nondeployed veterans, suggesting a potential healthy-warrior effect in which such conditions preclude deployment. Other neurologic conditions (e.g., brain tumor, Alzheimer’s disease/frontotemporal dementia) had a greater epilepsy impact in the deployed veterans. This may be attributable to deployment-related exposures (combat injury, occupational exposures).”
The study called for a better understanding of deployment effects, calling that “critical to provide targeted epilepsy prevention in veterans and military servicemembers.”
“While we found that the likelihood of epilepsy was significantly higher in veterans with traumatic brain injury, regardless of deployment status, the association of penetrating traumatic brain injury (where the skull and dura mater are penetrated) was significantly higher in those who deployed,” Pugh explained. “There was not a significant difference in the size of the association for mild traumatic brain injury, which accounted for over 80% of all traumatic brain injuries.”
“Moreover, some epilepsy predictors (moderate/severe traumatic brain injury, multiple sclerosis and Parkinson’s disease) were more strongly associated with epilepsy among those veterans who were not deployed,” she added. “This suggests there may be a healthy deployer effect, since those individuals with these types of risk factors are less likely to be deployed.”
The study authors suggested that, “although most neurologic conditions were more prevalent among the nondeployed veterans, they were often associated with higher odds of epilepsy in the deployed veterans.”
Pugh emphasized the importance of understanding a patient’s history of TBI.
“We know from our prior research that traumatic brain injury diagnosed in VA and DoD is limited and might not reflect the extent of traumatic brain injury that servicemembers and veterans experience,” she said. “That lifetime history is what is really important in understanding the impact of traumatic brain injury. Taking a comprehensive traumatic brain injury history would be beneficial for all service members and veterans if we are to truly understand long-term outcomes of traumatic brain injury.”
The authors noted that, “additional research that more closely examines the timing of conditions and injuries in deployed and non-deployed service members is needed to better understand the longitudinal nature of interactions between traumatic brain injury, deployment, and physical and psychiatric comorbidities.”
- Henion AK, Wang CP, Amuan M, Altalib HH, et. al. Role of Deployment History on the Association Between Epilepsy and Traumatic Brain Injury in Post-9/11 Era US Veterans. Neurology. 2023 Dec 12;101(24):e2571-e2584. doi: 10.1212/WNL.0000000000207943. Epub 2023 Nov 22. PMID: 38030395; PMCID: PMC10791059.
