SAN ANTONIO—No statistically significant racial differences in diffuse large B-cell lymphoma (DLBCL) outcomes were found for patients treated within the VHA, according to recent research.
“Our study highlights the significance of equal access system and that disease biology and other social factors can be mitigated resulting in equal response to treatment and OS amongst all groups,” according to the authors from the University of Texas Health and the South Texas Veterans Healthcare System, both in San Antonio, and colleagues.
The study presented at the recent American Society of Hematology’s 65 Annual Meeting and Exposition in San Diego noted that the incidence of DLBCL in the United Sates is projected to increase to 32,443 new cases per year by 2025.1
“With increasing incidence and prevalence, DLBCL prognosis has improved significantly in the past decade through the addition of novel therapies such as new monoclonal antibodies, chimeric antigen receptor T-cell (CAR-T) therapy, antibody-drug conjugates, and most recently bispecific T-cell engagers,” the researchers pointed out. “Despite these improvements, racial and ethnic disparities continue to impact outcomes in DLBCL patients.”
Source: Kaur S, Mader M, Franklin K, Williams M, et. cl. (2023, Dec. 9-12)
Examining Racial Disparities in Diffuse Large B-Cell Lymphoma (DLBCL) Outcomes within the Veterans Health Administration (VHA). 65th American Society of Hematology Annual Meeting and Exposition, San Diego, California.
The study team sought to assess racial and ethnic differences in DLBCL patients and outcomes within the VHA. Because VA healthcare is an equal-access system, confounding factors such as disease biology and socioeconomic status are more controlled. The authors suggested that provided them a better opportunity to examine racial disparities. The goal was to present a final analysis of racial and ethnic differences in DLBCL patients within the VHA over an 11-year period..
To do that, trained abstractors performed a retrospective chart review of 6,266 randomly selected DLBCL patients treated in the VHA nationwide between Jan. 1, 2011, and Dec. 31, 2021. All patients diagnosed with DLBCL were included. Excluded were patients who had a diagnosis other than DLBCL, had incomplete records or were diagnosed and treated outside the VHA.
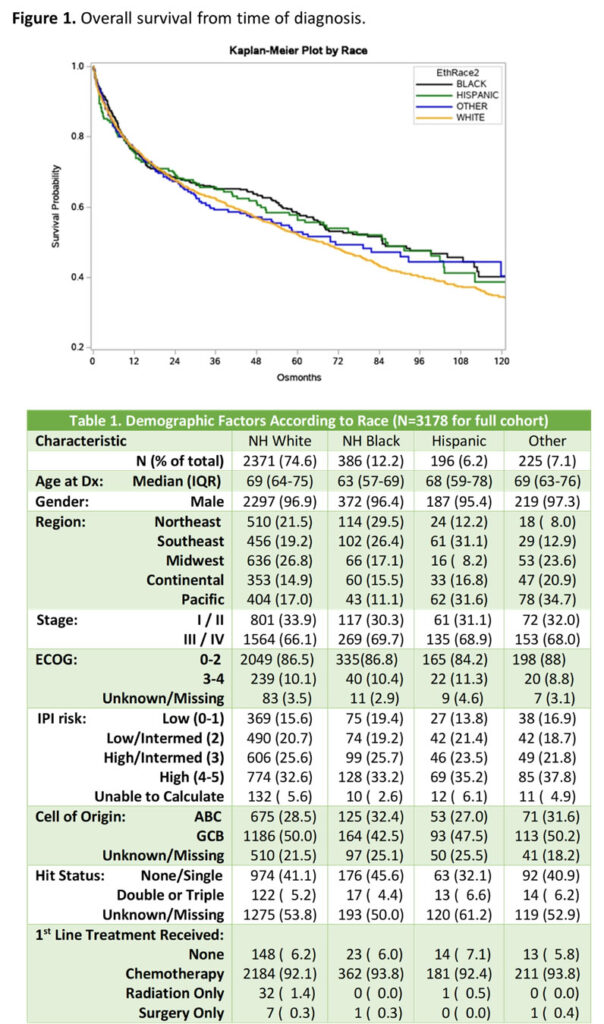
The researchers collected data on baseline patient demographics, disease characteristics and treatment. Survival time was determined via electronic health record query on Jan. 4, 2023. The investigators divided the study population into non-Hispanic Black (NHB), non-Hispanic white (NHW), Hispanic (H) and other.
Ultimately, 3,178 patients met inclusion criteria for analysis. Patients were predominantly male with a median age of 69 and presented primarily with advanced disease.
NHB were diagnosed at a younger median age (63 years) when compared to the NHW, H and other (69 years, P < 0.001), according to the findings. “Patients in each subgroup presented with similar rates of stage I/II and III/IV disease with no statistically significant difference in stage at presentation among each racial subgroup (P=0.61),” the researchers advised.
Results indicated that, of all the patients who received chemotherapy, the objective response (OR) rate was 79.2% with a complete response (CR) rate of 66.4%. “The response rates were similar across the four subgroups with most patients achieving a CR after first-line therapy (P=0.74). There were no statistically significant differences in OR rates amongst subgroups (P = 0.95),” according to the presentation.
The study found that median overall survival (mOS) for the entire population was 69.6 months (95% CI = 65-75), with a mOS of 85.1 months (67-112), 85.9 months (60-112), 67.4 months (60-73) and 71.2 months (49-122) for NHB, H, NHW, and other patients respectively. No statistically significant difference in mOS was identified among subgroups (P = 0.13). The 1-year, 3-year and 5-year survival rates were also similar between subgroups (P=0.97, P= 0.39, P=0.32, respectively), the authors added.
“This study represents one of the largest retrospective analyses of DLBCL in the VHA nationwide, highlighting that there is no statistically significant racial difference in DLBCL outcomes for patients treated within the VHA,” the researchers explained. “Our study highlights the significance of an equal access system and that disease biology and other social factors can be mitigated resulting in equal response to treatment and OS amongst all groups.”
They advised that their study had potential limitations, including the use of retrospective data on a predominantly white, male population that might not actually represent general DLBCL population data. The study period is mainly until 2021 with limited data on the accessibility of newer, novel treatments, the authors added.
“With the development of newer, expensive treatments, especially Bispecific T Cell Engagers and CAR-T therapy, it is imperative to study utilizations of these novel treatments and study racial differences in this new treatment non-chemotherapy-based era,” according to the researchers.
DLBCL is the most common non-Hodgkin lymphoma and accounts for 30% of all non-Hodgkin lymphoma cases, according to a previous VA study. It has an incidence of 5.6 per 100,000 persons per year in the United States.
The article in Future Oncology pointed out that a majority of patients are cured with first-line (1L) therapy that typically includes rituximab and an anthracycline-containing chemotherapy. Still, as many as 40% of patients are refractory to or relapse (R/R) after responding to initial treatment.2
Patients with R/R disease after 1L treatment who are eligible for bone marrow transplantation (BMT) receive an aggressive chemotherapy or chemoimmunotherapy (CT/CIT) regimen and, if responsive to CT/CIT, proceed to consolidative BMT, according to the authors from the George E. Wahlen VAMC and the University of Utah, both in Salt Lake City.
Some of those patients achieve long-term remissions, but those who do not respond, or who relapse after transplant, might receive further treatments of varying intensity.
- Kaur S, Mader M, Franklin K, Williams M, cl. (2023, Dec. 9-12)
Examining Racial Disparities in Diffuse Large B-Cell Lymphoma (DLBCL) Outcomes within the Veterans Health Administration (VHA). 65th American Society of Hematology Annual Meeting and Exposition, San Diego, California.
- Chien HC, Morreall D, Patil V, Rasmussen KM, et. al. i Real-world practice patterns and outcomes in Veterans with relapsed/refractory diffuse large B-cell lymphoma. Future Oncol. 2021 Feb;17(4):411-422. doi: 10.2217/fon-2020-0522. Epub 2020 Oct 29. PMID: 33115291.