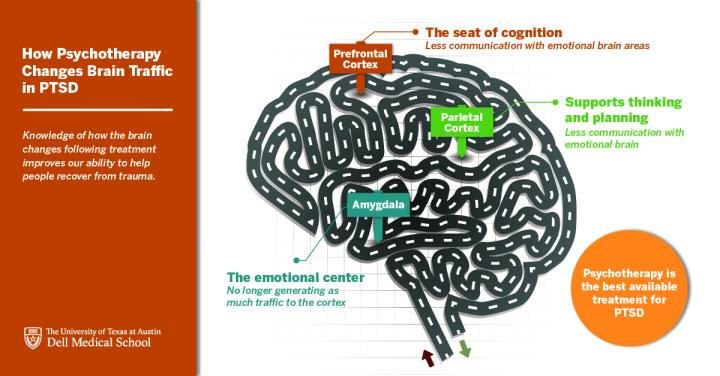
Click to Enlarge: Knowledge of how the brain changes following treatment improves our ability to help people recover from trauma. Source: University of Texas at Austin, Dell Medical School
WHITE RIVER JUNCTION, VT — Direct-acting antivirals used in the treatment of the hepatitis C virus might improve symptoms of post-traumatic stress disorder (PTSD), potentially offering a new therapeutic option for a prevalent disease with few approved medications, according to a new study.
The study, published in the journal Biological Psychiatry, analyzed large-scale electronic health record data to identify existing medications that may be repurposed as PTSD treatments. There are few medications approved by the U.S. Food and Drug Administration (FDA) for treatment, and approved medications do not work well enough.1
The researchers constructed a mechanistic tree of all FDA-approved medications and identified medications associated with greater-than-expected levels of clinically meaningful improvement in PTSD symptoms using electronic health record (EHR) data from the U.S. Department of Veterans Affairs. The study included 168,941 patients with a diagnosis of PTSD who had repeated symptom measurements using the PTSD Checklist over a 20-year period.
The researchers have been studying routine VA care for PTSD using medical records for many years. They had prior funding from the U.S. Department of Defense (DoD) to build a 20-year treatment cohort including over two million patients, which they used for this National Institutes of Health-funded study.
This study is the first large-scale exploration of existing medications that may have potential efficacy for the treatment of PTSD using a population-based sample. VA data are well-suited to the discovery of novel pharmaceutical treatments for PTSD for several reasons. First, PTSD is a common diagnosis among VA patients, and VA patients with PTSD have a high degree of medical comorbidity and receive a wide array of medications to address these illnesses. Second, the VA maintains national registry data sources capturing longitudinal patient care, including patient demographics, procedural and diagnostic codes, and pharmacy data, according to the study.
Meaningful Improvement
“We found that, in general, about 20% of patients with pre- / post-measurement of their PTSD symptoms experienced clinically meaningful improvement,” lead author Brian Shiner, MD, MPH, told U.S. Medicine. “That was our expected rate of improvement. We then calculated the rate of improvement for patients taking each FDA-approved medication. The observed to expected ratio for sertraline, which has an FDA indication for PTSD, was about 1.2. That means about 24% of patients who received sertraline had a meaningful improvement in their PTSD symptoms.”
Shiner is acting associate chief of staff for research for the White River Junction, VT, VAMC and associate professor at the Geisel School of Medicine at Dartmouth College in Hanover, NH.
“The observed to expected ratio for glecaprevir/pibrentasvir (GLE/PIB), which has an FDA indication for Hepatitis C Virus (HCV) infection, was about 2.2,” he said. “That means about 44%of patients who received GLE/PIB had a meaningful improvement in their PTSD symptoms. We were looking for this kind of signal for a possible off-target effect for a drug no one was thinking about for PTSD. In fact, we had never heard of GLE/PIB before it generated the strongest signal in our study.”
While some patients have great responses to available FDA-approved medications approved for PTSD, the research team’s previous work shows that many VA patients still have significant symptoms after an adequate course of sertraline or paroxetine.
Antidepressants, the most-prescribed pharmacologic agents for PTSD, are associated with remission in fewer than half of the patients who take them. Sertraline and paroxetine are currently the only antidepressants approved by the FDA to treat PTSD. The VA and DoD issued a treatment guideline that includes two additional antidepressant medications, fluoxetine and venlafaxine, that have similarly limited effectiveness.
There have been no new drugs approved by the FDA for the treatment of PTSD in almost two decades. Research and development of new drugs for PTSD have been limited, and current development might take many years to complete, so there’s a need to identify effective medications for PTSD treatment now.
“Hopefully many of those patients will access effective psychotherapies, such as cognitive processing therapy and prolonged exposure,” Shiner wrote in an email. “But some may also need a better medication, and our goal is to contribute to meeting that need through our work.”
The VA advised recently that about 11-20 out of every 100 veterans (or between 11-20%) who served in Operation Iraqi Freedom or Operation Enduring Freedom have PTSD in a given year. PTSD also affects approximately 3.5% of U.S. adults every year, according to the American Psychiatric Association. It was formally recognized as a diagnosis by the medical group in 1980, and there has been a great amount of research since then, from bench science to understand the biological causes of PTSD to development of standardized psychological assessments to help understand whether potential treatments work.
“I think a lot had to be in place for the field to mature. My hope is that we see more medication treatments coming down the pike in the coming years to supplement some of the great psychotherapy approaches that are already available,” Shiner wrote.
The study’s results are significant, because they offer another promising avenue for treatment development, which the researchers will pursue over the coming years. However, Shiner notes there are no clinical implications from the present study. The hepatitis C drug is a very expensive drug that has not been studied in patients without hepatitis C virus. At this stage, the results can’t be applied in practice.
“At this point, all we have is an exciting finding,” Shiner explained. “We have used VA data to look for medication that might be helpful for PTSD and found an interesting signal for a HCV medication. But there are many potential sources of bias in data mining, and we really need to investigate our signal with a prospective study in patients with PTSD who do not have HCV. Fortunately, we received funding from the DoD to conduct such a study at the White River Junction VA Medical Center. We are starting our open-label pilot study now and hope to start our randomized placebo-controlled trial by the spring.”
- Shiner B, Forehand JA, Rozema L, Kulldorff M, et. al. Mining Clinical Data for Novel Posttraumatic Stress Disorder Medications. Biol Psychiatry. 2022 Apr 1;91(7):647-657. doi: 10.1016/j.biopsych.2021.10.008. Epub 2021 Oct 20. PMID: 34952698; PMCID: PMC8918007.
