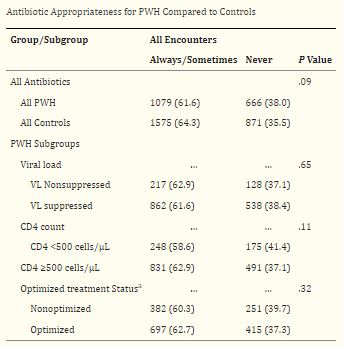
Click to Enlarge: Abbreviations: ARI, acute respiratory infection; ART, antiretroviral therapy; PWH, people with human immunodeficiency virus; VL, viral load.
a. Optimized treatment status defined as VL <200 copies/mL on ART with CD4 ≥500 cells/µL. All data expressed as number (%). Source: Open Forum Infectious Disease
FORT SAM HOUSTON, TX — Inappropriate antibiotic prescribing for acute respiratory infections, a major public health concern, is high in both patients with and without human immunodeficiency virus (HIV) and doesn’t appear to be affected by HIV status, according to a recent study.
The DoD HIV Virtual Cohort Study published in Open Forum Infectious Diseases assessed the incidence of acute respiratory infections and antibiotic prescribing for patients with HIV compared with HIV-negative controls because the data was limited.
The study authors included researchers from Brooke Army Medical Center at Fort Sam Houston, TX; and in Bethesda, MD, at the Uniformed Services University of the Health Sciences, Walter Reed National Military Medical Center and The Henry M. Jackson Foundation for the Advancement of Military Medicine Inc..1
The participants were a cohort of male military active-duty servicemembers and beneficiaries receiving care within the MHS since as early as 1997. Only males were included in this study because of the small number of females with HIV who were servicemembers or retirees, the study reported.
Included were 2,413 HIV patients and 4,827 controls, with about 45% identifying as African American. The two cohorts, patients with and without HIV, were matched by age, gender, race/ethnicity and beneficiary status. The analysis was conducted on a cohort level to better compare the influence of HIV status, rather than demographic features, a study author explained in an email.
“Overall, we found that people living with HIV appeared to have about as many outpatient visits for respiratory illness as those without HIV,” lead author Capt. Lauren Sweet, MD, chief of residents for internal medicine at Brooke Army Medical Center, told U.S. Medicine. “Unless their CD4 counts were depressed below 500 cells/uL or viral loads elevated, there were no significant differences between those with HIV and those without. Interestingly, those with HIV tended to receive antibiotics less often than those without HIV. However, that antibiotic was likely not necessary about one-third of the time for both patient populations.”
“Our analysis suggests that HIV status does not appear to increase visits for respiratory tract infection or inappropriate antibiotic prescribing compared with persons without HIV. We generally found high rates of inappropriate antibiotic prescribing for respiratory tract infections in all patients,” Sweet wrote.
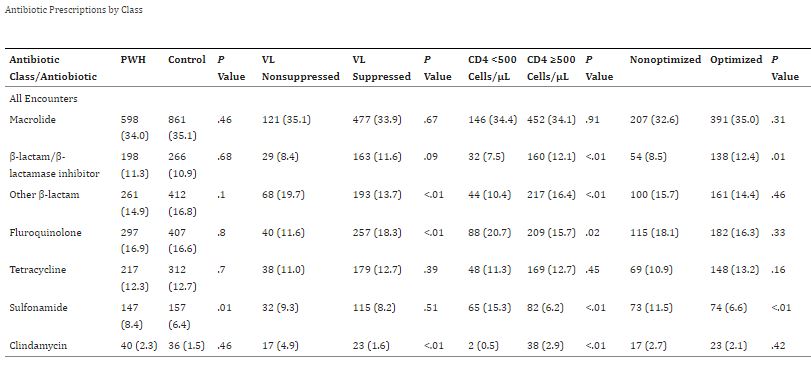
Click to Enlarge: Abbreviations: ART, antiretroviral therapy; PWH, people with human immunodeficiency virus; VL, viral load.
Notes: All data expressed as number (%). Percentages may not add up to 100 because some minor antibiotic classes were not included in this table. Source: Open Forum Infectious Disease
There is still “significant over usage of antibiotics in the outpatient setting, which does not appear to be affected by HIV status. The morbidity associated with antibiotic overuse for respiratory infections increases concerns for community antibiotic resistance and should be addressed on a systemic level,” Sweet added.
The study found that “antibiotics were prescribed in 26% of encounters among people with HIV, compared to 34% for controls.” Also, antibiotic use “was ‘never’ appropriate in 38% of encounters with people with HIV and 36% in controls. Compared to controls, people with HIV received more sulfonamides (5.5% vs. 2.7%), and variation existed among HIV subgroups in the prescription of sulfonamides, fluoroquinolones and β-lactams,” the study reported.
This study has “provided the largest analysis to date of the current prescription patterns among people with HIV. Understanding how prescribing patterns among people with HIV compare to the general population may allow for more targeted education to reduce antimicrobial exposure in a group that may already have higher rates of colonization with resistant organisms,” according to the study.
Antibiotic resistance is “an international health emergency that is driven by the inappropriate prescribing of antibiotics,” the authors pointed out. Previous studies in outpatient and acute-care populations have shown that as many as 50% of antibiotic prescriptions are inappropriate. Acute-respiratory infections in adults “are most likely to result in inappropriate prescribing and have the greatest value as a target for improvement in the reduction of inappropriate prescriptions,” the study explained.
Antibiotic Prescribing for Subpopulations
The prescribing rates for antibiotics during outpatient acute respiratory-infection encounters and the appropriateness for these prescriptions can vary for different settings. VA studies have shown that inappropriate antibiotic prescriptions for acute respiratory infections appear to be as high as 76%. Despite the need for improving guideline adherence, knowledge of prescribing patterns among subpopulations remains low and has mostly not been addressed, the study reported.
“Patient comorbidities have been shown to be a significant influencer of antibiotic prescribing practices, but many patients with comorbidities are frequently excluded from analyses,” the study noted, adding, “Because of concerns about immunosuppression and the common use of prophylactic antibiotics, people with HIV are often excluded from analyses of antibiotic prescriptions, and only sparse data on antibiotic prescribing for this population exists.”
The researchers offered some recommendations to healthcare professionals caring for patients with and without HIV infection who have acute respiratory-infection encounters. Their data suggest that “all providers within the system need to carefully evaluate their antibiotic use and ensure that all prescriptions adhere to guideline-based recommendations,” Sweet explained.
“Our initial concern was that uncertainty about the implications of the HIV status may have led to overprescribing antibiotics,” Sweet said. “We were able to analyze a very large population of individuals (several thousand) over five years (2016-2020) and note that our cohort of persons living with HIV are overall getting similar care for respiratory-tract infections as those without HIV. This may point to an overall shift in general attitudes in the comfort of treatment of persons living with HIV. Unfortunately, overprescribing was still common, reminding us of the distance still to go in antibiotic stewardship.”
The study suggested that “focused interventions to improve antibiotic appropriateness for prescribers caring for people with HIV should be pursued.”
- Sweet L, Daniels C, Xu X, Sunil T, Topal S, Chu X, Noiman A, Barsoumian A, Ganesan A, Agan BK, Okulicz JF. Acute Respiratory Infection Incidence and Outpatient Antibiotic Prescription Patterns in People With or Without Human Immunodeficiency Virus Infection: A Virtual Cohort Study. Open Forum Infect Dis. 2023 May 19;10(7):ofad272. doi: 10.1093/ofid/ofad272. PMID: 37476075; PMCID: PMC10354854.
