By: Jennifer Marquez
ORANGE, CT — Use of pre-exposure prophylaxis to prevent human immunodeficiency virus transmission remains relatively low for U.S. military servicemembers. New research suggests, however, that better understanding their treatment preferences could increase uptake.
Evidence shows that, when taken as prescribed, PrEP can be highly effective at preventing HIV, the researchers note. The U.S. military sees approximately 350 new HIV cases among its servicemembers every year. However, PrEP use among military members who are at highest risk for being diagnosed with HIV—which, as in civilian populations, include members who are younger, Black and men who have sex with men (MSM)—is low.
Furthermore, previous research has documented that just 16% of servicemembers who could benefit from PrEP use it, and the number is even lower among military personnel of color.1
The purpose of the study was to identify potential changes to the way PReP is administered within the U.S. military healthcare system that could increase use of the medication. A new survey of more than 400 U.S. military servicemembers was used to reveal PrEP preferences. 2
“Military members who become HIV-positive may face duty limitations related to their diagnosis and may not be eligible for certain assignments or deployments; thus affecting overall military readiness,” said David Vlahov, PhD, RN, one of the authors of the study and a professor at the Yale School of Nursing with a joint appointment in epidemiology and public health. “Therefore, it is important to address the low use of PrEP among military members to retain the talents and skills from our diverse military personnel to prevent an impact to military capabilities related to HIV infection.”
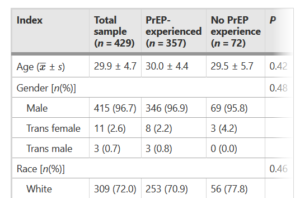
For the study, which was conducted anonymously, the researchers recruited HIV-negative, MSM service members through a closed lesbian, gay, bisexual and transgender (LGBT) military social media group. The 429 participants answered questions about their preferences for PrEP dosing method (such as a daily tablet or a yearly implant), provider type (civilian or military), visit and dispensing location (off-base, on-base or using a smartphone app), and lab work evaluation location (on-base, off-base or using a home-based mail kit).
Among the options presented, the most-preferred included a daily tablet, bimonthly PrEP injection or yearly implant, along with a military provider, smartphone/telehealth visit and on-base locations for lab evaluation and medication pickup.
A key preference factor was dosing method, with the majority of survey respondents preferring a daily tablet, which is the PrEP program currently available in the U.S. military healthcare system. Those with no previous experience taking PrEP also expressed interest in bimonthly injections and yearly implants. These longer-acting dosing methods also offer a benefit for military members who need to relocate, deploy, or miss regular follow-up appointments, the study notes.
“Dosing preferences within a PrEP program is important because there may be characteristics of an alternative PrEP dosing agent that better fit the HIV-protection needs of a military member,” said Vlahov. “For example, the military member who shares sleeping quarters with others may not want a bottle of PrEP pills to be visible for all to see, and may instead opt for a more discreet, longer-acting PrEP injection instead.” As newly developed injectable and alternative PrEP dosing agents transition toward real-world implementation, he added, these agents may provide a clear benefit over a daily tablet for individuals with pill fatigue, adherence or privacy concerns, or an unpredictable work schedule. Therefore, the availability of longer-acting and alternative PrEP dosing agents should be prioritized for military members to optimize PrEP uptake.
Although the survey reveals a preference for receiving PrEP from military healthcare providers, the study authors noted that these providers might need additional training and support to be comfortable prescribing the medication. A 2018 survey of military providers found that nearly half reported having poor knowledge of PrEP, and only 29% said that they had ever prescribed it, according to the MMWR article. Currently, 60% of military PrEP prescriptions are written after consultation with an infectious disease specialist, which also indicates that military providers may be uncomfortable prescribing PrEP.
“Given the legacy of ‘don’t ask, don’t tell, the since-repealed policy that once discharged military members for disclosing same-sex activity, some readers may be surprised to see an overall preference for a military provider within a PrEP program,” said Vlahov. “However, this is an encouraging finding, as it suggests that the military provider can be central to the success of a military PrEP program.”
The researchers also collected data on participants’ mental health, their objective risk for acquiring HIV based on recent behaviors, and their comfort level with talking about sex with a primary care providers. The survey found that nearly two-thirds of the participants reported symptoms of depression, and nearly 90% had engaged in behaviors (such as condomless sex) that put them at high risk for HIV. More than a third of respondents said that they were uncomfortable bringing up sex with their doctors.
“Discomfort discussing sex with primary care providers may stem from the historical precedent of ‘don’t ask, don’t tell,’” said Vlahov. He also said that there are other barriers to PReP use among service members. For example, “some positions within the military (e.g., aviation, undersea) may require special waivers to be on PrEP, thus potentially requiring further disclosures of same-sex activity with additional entities outside of the healthcare environment. Therefore, some at-risk military members who may prefer to have more discretion regarding their sexual history and activity may not want to embark on these additional steps to obtain PrEP.”
The study authors pointed out that, as more and more evidence suggests a link between depression and sexual risk behaviors among MSM, it may be beneficial to provide access to PrEP clinics that are both sensitive and inclusive to sexual identity and vigilant to address factors related to mental and sexual health. The authors say they hope that the study can help develop better training for military healthcare providers on medication regimens.
“Knowing preferences is a starting point in behavior change. We need to learn how preferences translate into practice,” Vlahov said.
- Blaylock JM, Hakre S, Okulicz JF, et al. HIV preexposure prophylaxis in the U.S. military services – 2014-2016. Morbidity and Mortality Weekly Report (MMWR). Published May 25, 2018. DOI: 10.15585/mmwr.mm6720a1.
- Gutierrez, JI, Dubov A, Altice FL, Vlahov D. Preferences for pre-exposure prophylaxis among U.S. military men who have sex with men: results of an adaptive choice based conjoint analysis study. Military Medical Research. Published May 19, 2021. DOI: 10.1186/s40779-021-00323-6.