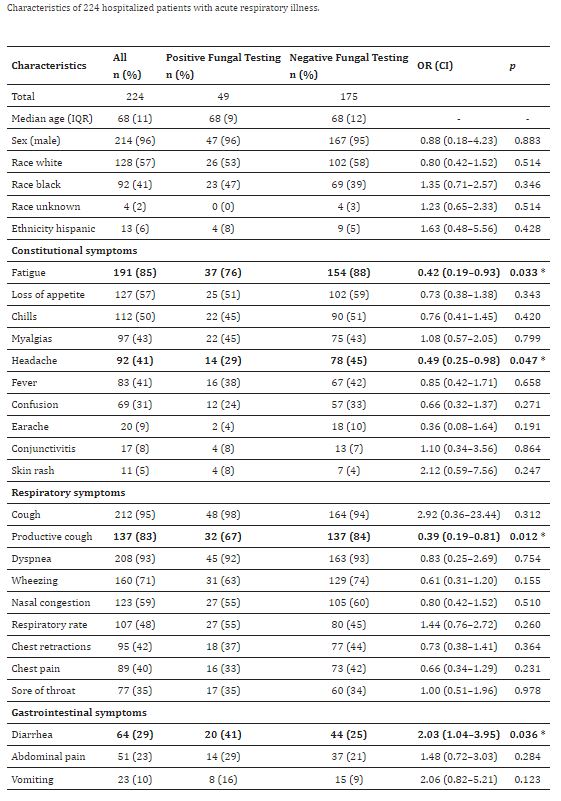
Click to Enlarge: Negative viral testing: respiratory specimens that tested negative using approved BioFire (BioFire Diagnostics, LLC, Salt Lake City, UT, USA) for respiratory pathogens, including influenza, RSV, parainfluenza, human metapneumovirus, rhinoviruses/enteroviruses, and adenovirus. (*) p < 0.05, OR: odds ratio, CI: 95% confidence interval. Source: Journal of Fungi
HOUSTON — Fungal infections are known to be causes of community-acquired pneumonia (CAP) and acute respiratory illness (ARI), but it is not clear how their frequency compares with that of viral and bacterial causes of these conditions. Although it is rarely possible to distinguish between fungal and other causes of infection, fungal infections are not often tested for by clinicians who care for ARI or CAP patients.
A new study published in the Journal of Fungi (Basel, Switzerland) suggests that, among patients hospitalized for ARI, fungal infections might be more common than previously thought and that testing for these could lead to more prompt and appropriate treatment.1
To examine the prevalence of positive fungal immunodiagnostics for often-overlooked fungal diseases as potential causes of ARI in hospitalized patients with negative viral or bacterial testing, researchers performed fungal testing on serum specimens from patients hospitalized with acute respiratory illness. The study enrolled patients hospitalized with ARI at the hospital Michael E. DeBakey VAMC in Houston from, November 2016-August 2017.
“ARI was defined broadly,” the authors wrote, and patients were eligible for inclusion if they were admitted for less than 72 hours with any of the following symptoms and syndromes:
- Influenza-like disease, influenza, upper respiratory infection (URI), viral URI, cough or bronchitis;
- Pneumonia, bacterial pneumonia, community-acquired pneumonia, aspiration pneumonia, rule-out pneumonia, evaluate pneumonia or bibasilar pneumonia;
- Chronic obstructive pulmonary disease (COPD) exacerbation, asthma exacerbation, status asthmaticus or asthmatic bronchitis;
- Acute respiratory distress syndrome (ARDS), fever, nasal congestion, chest congestion, sore throat, chills, body aches/myalgias, fatigue, respiratory distress, shortness of breath, difficulty in breathing, dyspnea, sepsis, cystic fibrosis exacerbation, respiratory medical other, congestive heart failure, idiopathic pulmonary fibrosis, altered mental status and new onset, exacerbation or change of two or more of the following symptoms with at least one respiratory symptom beginning less than 10 days;
- Respiratory symptoms: cough, shortness of breath, nasal congestion, chest congestion or sore throat;
- Constitutional symptoms: fever/feverishness, chills, body aches/myalgias or fatigue.
Epidemiologic and clinical data, nasopharyngeal and oropharyngeal samples for viral testing (PCR) and serum specimens were collected at admission. The researchers retrospectively tested remnant sera from a subset of patients with negative initial viral testing using immunoassays for the detection of Coccidioides and Histoplasma antibodies (Ab) and Cryptococcus, Aspergillus and Histoplasma antigens (Ag).
Of 224 patient serum specimens tested, 49 (22%) had positive results for fungal pathogens, the study found. This included 30 (13%) by Coccidioides immunodiagnostic assays, 19 (8%) by Histoplasma immunodiagnostic assays, 2 (1%) by Aspergillus Ag, and none by Cryptococcus Ag testing.
“A high proportion of veterans hospitalized with ARI had positive serological results for fungal pathogens, primarily endemic mycoses, which cause fungal pneumonia,” the researchers wrote. “The high proportion of Coccidioides positivity is unexpected as this fungus is not thought to be common in southeastern Texas or metropolitan Houston, though is known to be endemic in southwestern Texas.”
The authors stated their report has several limitations, particularly the potential for false positives and cross-reactivity, as well as the inability to determine whether fungal infections, when present, were the cause of the patients’ symptoms. In addition, the study included only a single medical institution, which limited the generalizability of the results. Also, because the researchers did not have access to paired specimens, they could not evaluate immune conversion, resulting in lower specificity.
Despite these limitations, they said their findings suggest that fungal infections might be more common than appreciated in ARI, particularly since viral or bacterial etiologies were not identified in most cases.
“It highlights the importance for clinicians to consider and test for fungal diseases in patients with ARI, especially for those who test negative for viral or bacterial infections, to increase timely treatment and to reduce inappropriate use of antibiotics,” they wrote. “The best diagnostic testing modality in this setting needs to be further evaluated.”
- Caceres DH, Rodriguez-Barradas MC, Whitaker M, Jackson BR, et. al. Fungal Pathogens as Causes of Acute Respiratory Illness in Hospitalized Veterans: Frequency of Fungal Positive Test Results Using Rapid Immunodiagnostic Assays. J Fungi (Basel). 2023 Apr 8;9(4):456. doi: 10.3390/jof9040456. PMID: 37108910; PMCID: PMC10145596.

