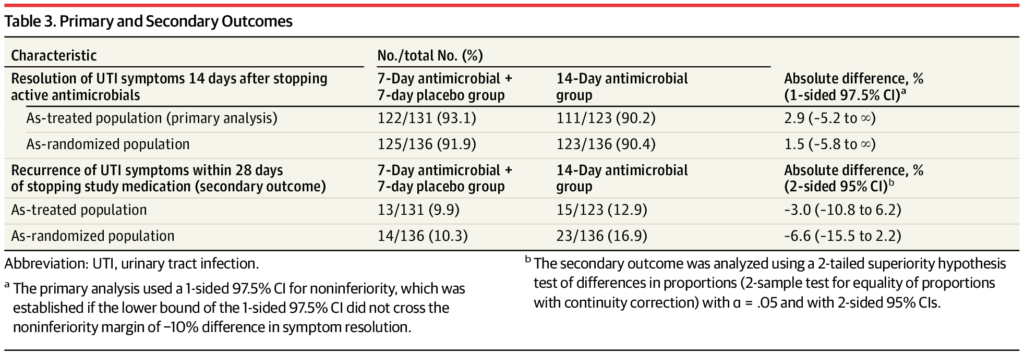
Click to Enlarge: a The primary analysis used a 1-sided 97.5% CI for noninferiority, which was established if the lower bound of the 1-sided 97.5% CI did not cross the noninferiority margin of −10% difference in symptom resolution.
b The secondary outcome was analyzed using a 2-tailed superiority hypothesis test of differences in proportions (2-sample test for equality of proportions with continuity correction) with α = .05 and with 2-sided 95% CIs.
MINNEAPOLIS — Urinary tract infection is one of the diagnoses for which antibiotics are most commonly used. So, a study determining that shorter duration treatment works as well as a longer course of antibiotics can have an outsized effect on reducing overuse of antimicrobials.
That is especially the case for agents active against gram-negative bacteria, where emerging resistance is of great concern, according to a new veterans’ study.
Another VA study signaled that the issue can be a double-edged sword, however, and demonstrated that suboptimal antibiotic use for UTIs in veterans in long-term care can be harmful.
A report in JAMA raised the question of whether men with symptoms of urinary tract infection (UTI) who are afebrile could be adequately treated with ciprofloxacin or trimethoprim/sulfamethoxazole for seven days, instead of the usual 14 days prescribed to resolve UTI symptoms.1
Minneapolis VA Health Care System-led researchers conducted a randomized clinical trial including 272 men with presumed symptomatic UTI to provide an answer. Results indicated that resolution of initial UTI symptoms by 14 days after completion of antibiotic therapy occurred in 122 of 131 (93.1%) of participants in the 7-day group and 111 of 123 (90.2%) in the 14-day group. That difference met the prespecified noninferiority margin of 10%, according to the authors.
Also participating in the study were researchers from the University of Minnesota Medical School in Minneapolis, and the Michael E. DeBakey VAMC and the Baylor College of Medicine, both in Houston.
The authors advised that their findings support the use of a 7-day course of ciprofloxacin or trimethoprim/sulfamethoxazole as a substitute to a 14-day course for the treatment of afebrile men with suspected UTI.
“Determination of optimal treatment durations for common infectious diseases is an important strategy to preserve antibiotic effectiveness,” they emphasized.
The randomized, double-blind, placebo-controlled noninferiority trial, reported in JAMA, was conducted at two VAMCs, with enrollment from April 2014 through December 2019 and final follow-up on Jan. 28, 2020. Of 1058 eligible veterans, 272 were randomized as trial participants.
For the study, patients were instructed to continue the antibiotic prescribed by their treating clinician for 7 days of treatment, and then half were randomized to receive continued antibiotic therapy—the other half got a placebo—for days 8 to 14 of treatment.
The authors noted that recurrence of UTI symptoms occurred in fewer than 10% of participants in the 7-day group vs. 12.9% in the 14-day group (difference, -3.0% [95% CI, -10.8% to 6.2%]; P =0.70), while adverse event rates were lower in the 7-day group, 20.6%, vs. the 14-da group, 24.3%.
“Among afebrile men with suspected UTI, treatment with ciprofloxacin or trimethoprim/sulfamethoxazole for 7 days was noninferior to 14 days of treatment with regard to resolution of UTI symptoms by 14 days after antibiotic therapy,” the researchers concluded. “The findings support the use of a 7-day course of ciprofloxacin or trimethoprim/sulfamethoxazole as an alternative to a 14-day course for treatment of afebrile men with UTI.”
Optimal Duration
The study was especially important, the authors wrote, because “determining the optimal treatment duration for common infectious diseases is an important strategy to preserve the effectiveness of antimicrobials. A growing body of evidence has shown that shorter-duration treatment performed similarly to longer-duration treatment for many infections, including pneumonia, intra-abdominal infections, osteomyelitis, cellulitis, urinary tract infection (UTI) in women and others. These findings support prescribing antimicrobials for no longer than needed to resolve manifestations of infection, given that extended treatment often does not provide additional benefit, is costly and inconvenient, and increases the risk of adverse events.”
Another recent VA study looked at the flip-side of the issue with treating UTIs: suboptimal use of antibiotics.
Researchers from the Providence, RI, VAMC and the University of Rhode Island pointed out, “Antibiotic use is associated with several antibiotic-related harms in vulnerable, older long-term care (LTC) residents. Suboptimal antibiotic use may also be associated with harms but has not yet been investigated.”
The study team sought to compare rates of poor clinical outcomes among LTC residents with UTI receiving suboptimal vs. optimal antibiotic treatment. To do that, researchers conducted a retrospective cohort study among residents with an incident urinary tract infection (UTI) treated in VA LTC units between 2013-2018.
The study defined potentially suboptimal antibiotic treatment as use of a suboptimal initial antibiotic drug choice, dose frequency and/or excessive treatment duration. Researchers were focused on time to a composite measure of poor clinical outcome, defined as UTI recurrence, acute care hospitalization/emergency department visit, adverse drug event, Clostridioides difficile infection (CDI) or death within 30 days of antibiotic discontinuation.
Results published in BMC Geriatrics found that, among 19,701 LTC residents with an incident UTI, 64.6% received potentially suboptimal antibiotic treatment and 35.4% experienced a poor clinical outcome After adjusted analyses, researchers determined that potentially suboptimal antibiotic treatment was associated with a small increased hazard of poor clinical outcome (aHR 1.06, 95% CI 1.01-1.11) as compared with optimal treatment, driven by an increased hazard of CDI (aHR 1.94, 95% CI 1.54-2.44).2
“In this national cohort study, suboptimal antibiotic treatment was associated with a 6% increased risk of the composite measure of poor clinical outcomes, in particular, a 94% increased risk of CDI. Beyond the decision to use antibiotics, clinicians should also consider the potential harms of suboptimal treatment choices with regards to drug type, dose frequency, and duration used,” the authors wrote.
They pointed out that, while prior studies have assessed the harms associated with unnecessary antibiotic use, “no previous studies have assessed the harms associated with suboptimal antibiotic use, whether or not the antibiotics were necessary or unnecessary. Suboptimal antibiotic treatment as assessed by drug choice, dose, and/or duration, in already frail, older residents could also be associated with other poor clinical outcomes such as infection recurrence, acute care hospitalizations, visits to the emergency department, or even mortality.”
- Drekonja DM, Trautner B, Amundson C, Kuskowski M, Johnson JR. Effect of 7 vs 14 Days of Antibiotic Therapy on Resolution of Symptoms Among Afebrile Men With Urinary Tract Infection: A Randomized Clinical Trial. JAMA. 2021;326(4):324–331. doi:10.1001/jama.2021.9899
- Appaneal HJ, Shireman TI, Lopes VV, Mor V, Dosa DM, LaPlante KL, Caffrey AR. Poor clinical outcomes associated with suboptimal antibiotic treatment among older long-term care facility residents with urinary tract infection: a retrospective cohort study. BMC Geriatr. 2021 Jul 23;21(1):436. doi: 10.1186/s12877-021-02378-5. PMID: 34301192.
