TUSCALOOSA, AL — PTSD can have a profound effect on quality of life and emotional well-being. Symptoms such as nightmares, difficulty sleeping or concentrating, as well as thoughts of self-harm can continue or reemerge throughout life. Veterans with PTSD may report troublesome symptoms 50 years or more after their wartime experience.
A new study shows the economic burden of PTSD, too, is immense—a finding which VA researcher Lori Davis, PhD, said she hopes will lead to greater public and private investment into better treatments for the condition.
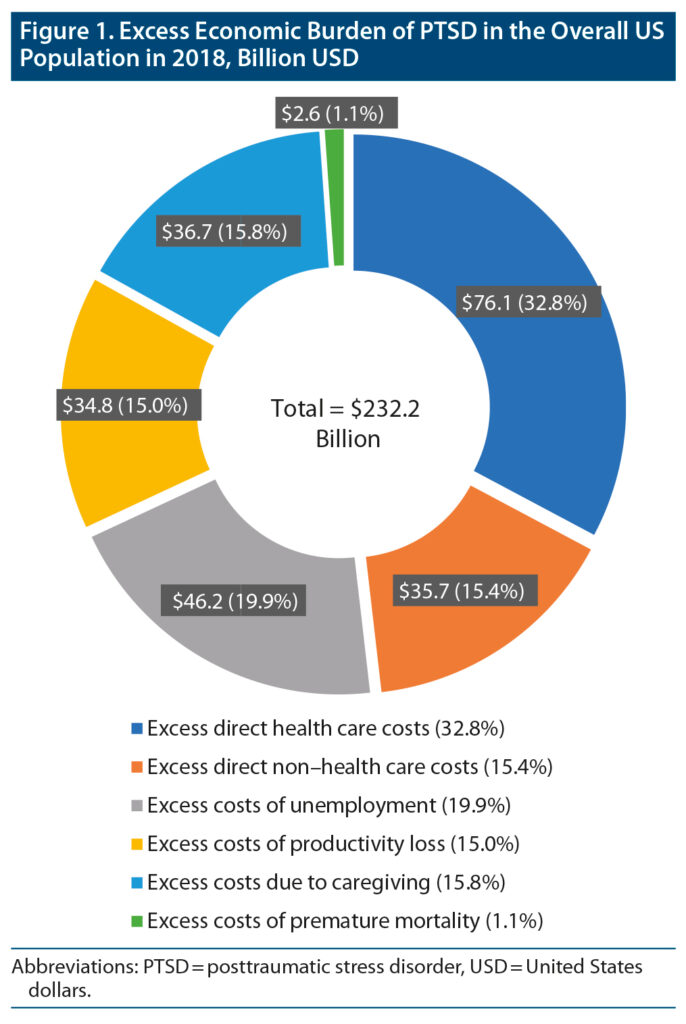
In 2018, the most recent year for which data were available at the time of the study, the cost of PTSD in both veterans and non-veterans was a “staggering” $232.2 billion, said Davis, associate chief of staff for research at the Tuscaloosa VA Medical Center in Alabama and the study’s lead author. The cost goes beyond direct healthcare expenses and exceeds the costs of other common mental health conditions, such as anxiety and depression, she said. 1
Davis, whose 28-year VA career has been focused on the prevention and treatment of PTSD, led the study as a way to “really understand the scope of the problem,” she said.
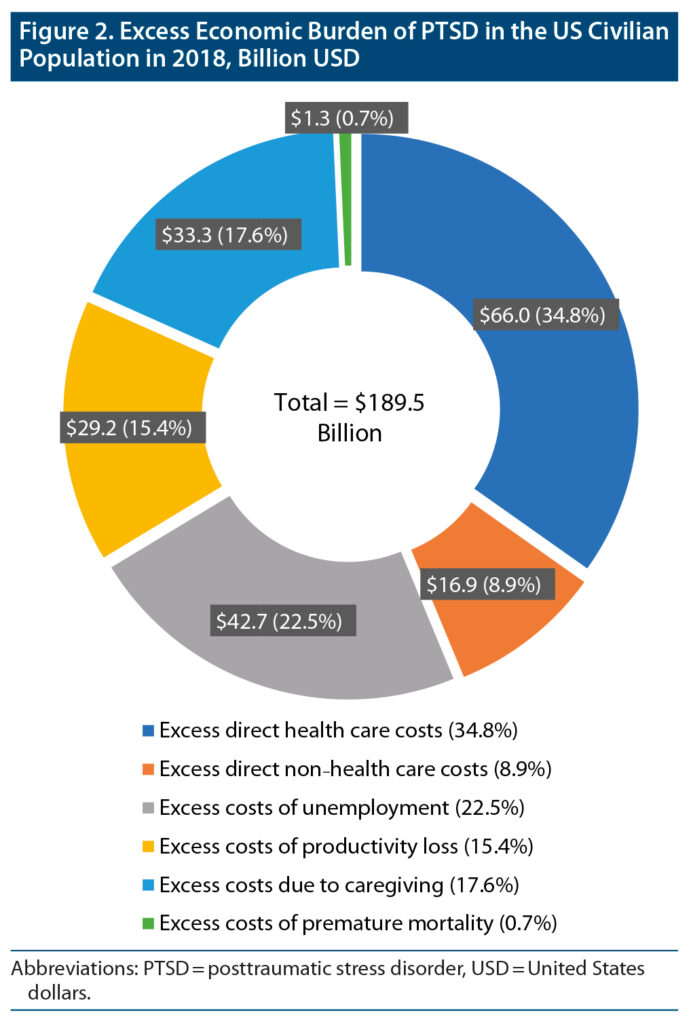
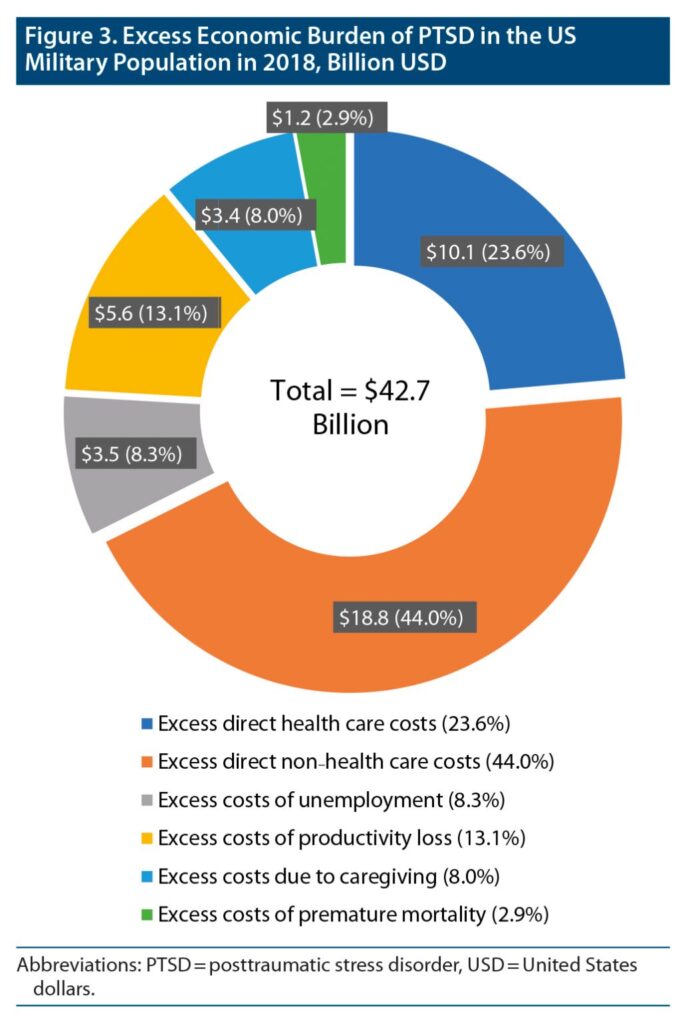
She and her team used insurance claims data, academic literature and government publications to estimate the costs of PTSD in both the US civilian and military populations, which included both active-duty military and veterans. They compared excess direct healthcare costs (pharmacy, medical), direct non-healthcare costs (research and training, substance use, psychotherapy, homelessness, disability) and indirect costs (unemployment, productivity loss, caregiving, premature mortality) associated with PTSD between adults with PTSD and adults without PTSD, or the general population if information was not available for adults without PTSD.
Key findings of the study included:
- The total excess burden of PTSD averaged $19,630 per individual with PTSD. (For civilians the average was $18,640; for the military population the average was $25,684 per individual with PTSD.)
- In the civilian population, the excess burden was driven by direct healthcare ($66.0 billion) and unemployment ($42.7 billion) costs.
- In the military population, the excess burden was driven by disability ($17.8 billion) and direct healthcare ($10.1 billion) costs.
“Direct health care costs were only about a third of the society harm, which was surprising,” said Davis. Larger non-direct costs included unemployment, which represented about 20% of the cost and loss of productivity, which accounted for 15%, she said. A fraction of the cost was premature immortality.
Also surprising to Davis was the scope of the problem in the nonmilitary. “There are more civilians in the US population than veterans, so you have more individuals in the civilian bucket adding to the cost,” she said, adding this was justification for the public and private sector—not only the VA and Department of Defense—to fund more research into the problem.
“You have to make a business case for the illness that you are trying to change the trajectory of recovery for,” she continued. “This is part of the business case for the seriousness of the disorder that this affects us all in the United States—citizens and veterans, taxpayers and family members. It kind of puts a dollar amount on it, and it seems as if we live in the world where the cost of things and the price tag gets people’s attention. This was a very careful and conservative modeling for the cost. If anything, it may be an under-estimate. It is a conservative estimate of the cost to the United States for the illness of PTSD, and it is staggering.”
Davis said she believes that better access to healthcare could have meant a higher direct healthcare costs but would have reduced the productivity loss, unemployment or disability. “I think we can try to decide the strategy going forward and see if you invest more in good healthcare and evidence-based treatments, if you invest more in research to develop novel and effective treatments, then can you reduce the disability, unemployment, productivity loss and caregiving costs.”
“The next step is an analysis of what is the price tag of improved quality of life that would come from that access to treatment and development of more effective treatments,” she said. “You are going to improve the quality of life, reduce the non-direct healthcare burden, and therefore the cost would be offset by better quality of life.”
- Davis LL, Schein J, Cloutier M, Gagnon-Sanschagrin P, Maitland J, Urganus A, Guerin A, Lefebvre P, Houle CR. The Economic Burden of Posttraumatic Stress Disorder in the United States From a Societal Perspective. J Clin Psychiatry. 2022 Apr 25;83(3):21m14116. doi: 10.4088/JCP.21m14116. PMID: 35485933.