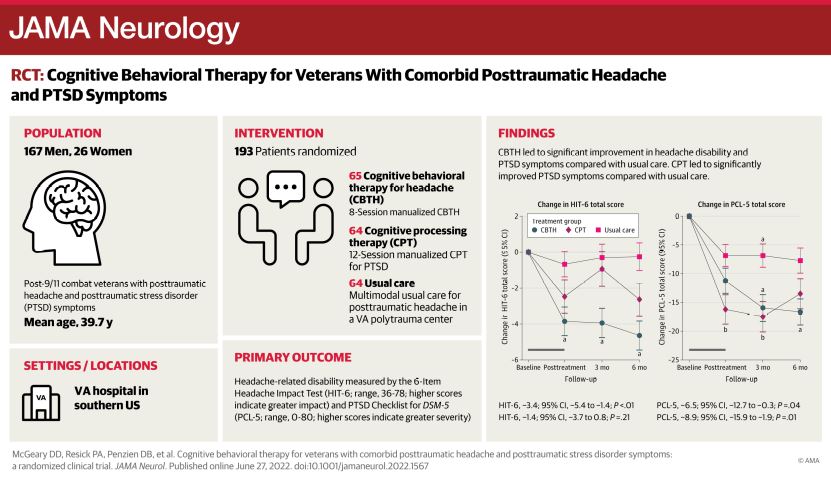
Click To Enlarge: Cognitive Behavioral Therapy for Veterans With Comorbid Posttraumatic Headache and PTSD Symptoms Source: JAMA Neurology
SAN ANTONIO — Military servicemembers and veterans are at high risk for head injury compared with civilians. More than 369,000 U.S. veterans have at least one mild traumatic brain injury, and many report the onset or worsening of headache within three months of their injury.
For many of them pain is complicated by comorbidities like post-traumatic stress disorder, depression and insomnia, and with each comorbidity the pain becomes more intense and more difficult to treat, said Don McGeary, PhD, research health scientist at the South Texas Veterans Health Care System in San Antonio and lead author of a new study evaluating the first therapy developed specifically for traumatic headaches—cognitive behavioral therapy for headache (CBTH).
McGeary and his colleagues developed CBTH by modifying a psychotherapy for migraine headaches, which uses cognitive behavioral therapy concepts to reduce headache disability and improve mood. CBTH includes key components such as relaxation, setting goals for activities patients want to resume, and planning for those situations. The new study, which was published in JAMA Neurology, found that CBTH not only significantly reduced related disability in veterans following a traumatic brain injury, but it also reduced co-occurring symptoms of PTSD comparably to the gold-standard PTSD treatment.1
Funded as part of the Consortium to Alleviate PTSD—a group jointly funded by the Departments of Defense and VA—the study was a single-site, 3-parallel group, randomized clinical trial with outcomes at post-treatment, 3-month follow-up, and 6-month follow-up. Participants were enrolled from May 1, 2015, through May 30, 2019, and post-9/11 U.S. combat veterans from multiple trauma centers were included in the study. Veterans had comorbid post-traumatic headache and PTSD symptoms.
“Because we were testing a brand-new treatment, we decided to focus on one recruitment and treatment site,” McGeary told U.S. Medicine. “We also decided to be flexible with how we defined ‘post-traumatic headache’ for this study.” At present, a person needs to report headache within seven days of a head injury for it to be considered “post-traumatic,” but many servicemembers who are exposed to a blast injury won’t see a specialist physician for months, he explained. For that reason, the researchers expanded the definition of post-traumatic headache to a headache that occurs within three months of head injury. Once selected for the study, veterans were asked to complete assessments about their headache, mood and PTSD and were randomly assigned to CBTH, a gold standard treatment for PTSD (cognitive processing therapy, CPT), or usual care in a VA Polytrauma Rehabilitation Center, he said.
Co–primary outcomes were headache-related disability on the six-Item Headache Impact Test (HIT-6) and PTSD symptom severity on the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders (Fifth Edition) (PCL-5) assessed from treatment completion to six months post-treatment.
Surprising Success
There were two key findings, said McGeary. “First, the headache intervention worked better than expected, and the effects of this brief intervention lasted for at least six months after treatment ended,” he said. “That was a big surprise, because this is one of the first trials to confirm the efficacy of CBT for this kind of headaches. Second, we compared CBTH to a gold-standard PTSD intervention and found that CBTH offered similar significant improvement in PTSD symptoms compared to the gold standard treatment despite not addressing PTSD at all. This is particularly notable, because CBTH is much briefer and easier for veterans to complete than the PTSD treatment.”
McGeary, who has treated and studied military servicemembers and veterans since 2003, said his motivation to develop and study the new treatment was that most current pain treatments used, including migraine medications, focused solely on pain. “I have become increasingly interested in figuring out how to address pain and trauma comorbidities concurrently to deliver the best care to our service members and veterans,” he said.
A significant lesson learned from the trial is that complex conditions such as headache with comorbid traumatic brain injury and PTSD do not need complex interventions, McGeary said. “The CBT intervention for this study was brief—about 4-5 hours of treatment— and simple to use,” he said. “Veterans with headache learned about stress management, relaxation, trigger management and problem-solving. For example, simply planning for an outing with the family—such as bringing sunglasses to prevent bright light from worsening a headache, packing a cold compress to help any headache that develops—can significantly improve the quality of that family time, and distraction with meaningful activity makes headache pain more manageable.”
- McGeary DD, Resick PA, Penzien DB, McGeary CA, et. al. Cognitive Behavioral Therapy for Veterans With Comorbid Post-traumatic Headache and Post-traumatic Stress Disorder Symptoms: A Randomized Clinical Trial. JAMA Neurol. 2022 Jun 27:e221567. doi: 10.1001/jamaneurol.2022.1567. Epub ahead of print. PMID: 35759281; PMCID: PMC9237802.
