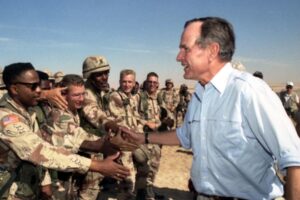
President George H.W. Bush met with troops in Saudi Arabia on Thanksgiving during the Gulf War, Nov. 22, 1990. Now researchers are trying to determine why veterans of that war so often develop chronic pain. DoD photo
Gulf War veterans with chronic pain display changes in the volume of key areas of the brain, a finding that could explain why these veterans experience prolonged pain, according to a new study.
The study published in The Journal of Neuroscience found Gulf War veterans with chronic musculoskeletal pain had smaller gray-matter volumes within a critical brain region of the descending pain processing network and larger volumes within brain regions associated with pain sensation and affective processing, which might reflect their transition of pain from acute to chronic pain.i
The researchers evaluated gray-matter volumes and associations with symptoms, physical activity and sedentary time in Gulf War veterans with and without chronic musculoskeletal pain. Data for this study were collected across three separate VA facilities—one in East Orange, NJ, and two in Madison, WI.
The participants were 98 Gulf War veterans (10 females) with chronic musculoskeletal pain and 56 Gulf War control veterans (7 females) who completed T1 weighted magnetic resonance imaging, pain and fatigue symptom questionnaires and physical activity measurement via actigraphy. Veterans were excluded from the study for a number of reasons, including current use of certain prescription pain medications and the presence of neurological disorders or mental health diagnoses that might affect brain morphology.
Chronic pain is a primary feature of Gulf War illness, a disease that affects nearly 35% of veterans who were deployed to the Persian Gulf War and is characterized by clusters of symptoms, such as pain, fatigue, problems with concentration and memory, respiratory disorders and gastrointestinal issues. Chronic musculoskeletal pain is a significant burden for these veterans, but the causes are poorly understood. Also, brain structure abnormalities are observed in Gulf War veterans, but relationships with modifiable lifestyle factors such as physical activity are unknown.
“Our most meaningful findings were that Gulf War veterans with chronic musculoskeletal pain have smaller brain volumes in a critical pain-regulation region of the brain, the insula, that is significantly related to their symptoms, and larger brain volumes in a diverse set of frontal-lobe brain regions involved in the cognitive affective aspects of pain processing and suggestive of pain amplification,” Dane B. Cook, PhD, told U.S. Medicine.
“When considering the Gulf War veterans’ widespread musculoskeletal pain symptoms, the brain volume literature from civilians with chronic widespread pain and fibromyalgia, and the regional brain differences that we observed, these results suggest that central nervous system dysregulation of pain processing (i.e., central sensitization) may be present in Gulf War veterans with chronic musculoskeletal pain and contributing to their symptoms. If confirmed, interventions that are aimed at reducing central sensitization could be explored as viable treatments for veterans with Gulf War illness where chronic widespread pain is a primary symptom,” according to Cook, senior author of the study and professor in the Department of Kinesiology at the University of Wisconsin-Madison and William S. Middleton Memorial Veterans Hospital, also in Madison.
Effective Treatments
The results are significant, because determining the pathophysiology of chronic muscle pain in Gulf War veterans is critical for designing effective treatments.
“As we learn more about the brain in disease, and chronic pain specifically, we are realizing that it is much more plastic (i.e., can change) than previously thought,” Cook explained. “Thus, treatments that can improve brain health may improve chronic pain by improving pain regulation mechanisms.”
These treatments also could improve other symptoms of Gulf War illness, which is important because Gulf War veterans with chronic pain also report worse mood, fatigue and physical function and engage in less physical activity than otherwise healthy Gulf War veterans. Chronic pain is associated with both biological and behavioral outcomes that negatively affect quality of life.
The findings also provide critical evidence that the brains of symptomatic Gulf War veterans are different from otherwise healthy deployed veterans, and importantly, that these differences were significantly related to their symptoms. The results are further strengthened by the study’s requirement that all participants had been deployed to the Gulf War, and veterans with chronic pain had to report experiencing pain in three or more quadrants of the body for more than three months. Many veterans had experienced their pain for many years. These criteria make the results more specific to Gulf War veterans who experience chronic muscle pain as their primary disease, Cook wrote.
Despite the findings, the study doesn’t conclude the brain structure of these veterans changed because of their experience in the Gulf War.
“We cannot make any claims that deployment and service in the Gulf War caused the differences in brain volumes that we observed,” Cook told U.S. Medicine. “This study was cross-sectional, meaning it is one snapshot in time, and thus we can only say that the differences in brain volumes that we observed are associated with service during the Gulf War. Longitudinal designs where we track brain volumes, symptoms and other behaviors over time, or interventions designed to improve brain health, would be necessary to begin to make claims of causation. This does not mean that these results are not important. They certainly are, but we need to be cautious in the claims that we make.”
Cook added that more research focused on the brain health of Gulf War veterans is needed, particularly research that employs longitudinal monitoring and treatment trials utilizing multimodal neuroimaging methods to better understand how central nervous dysregulation occurs either as a result or as a precipitating factor of Gulf War illness.
- Ninneman JV, Gretzon NP, Stegner AJ, Lindheimer JB, Falvo MJ, Wylie G, Dougherty RJ, Almassi NE, Van Riper SM, Boruch AE, Dean DC 3rd, Koltyn KF, Cook DB. Pain, but not Physical Activity, is Associated with Gray Matter Volume Differences in Gulf War Veterans with Chronic Pain. J Neurosci. 2022 Jun 13:JN-RM-2394-21. doi: 10.1523/JNEUROSCI.2394-21.2022. Epub ahead of print. PMID: 35697521.

