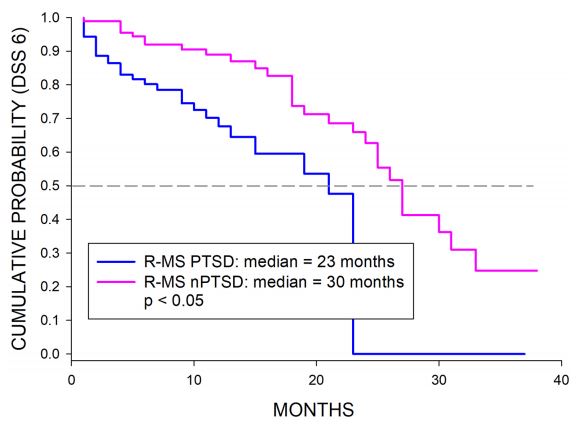
Click to Enlarge: The graph represents the Kaplan–Meier survival functions for disability progression to DSS 6.0 for MSPTSD and MS control groups for MS with relapsing onset (RMS). Source: Multiple Sclerosis Journal
BALTIMORE — An unfortunate confluence of events puts a significant number of veterans at higher risk of both multiple sclerosis and post-traumatic stress disorder (PSTSD). Agent Orange and other exposures make multiple sclerosis (MS) a presumptive condition for those who have served, while combat experience, higher rates of sexual assault and other factors increase the likelihood of PTSD among veterans.
While the impact of mental health on many physical illnesses has been well documented, little research has been conducted on the interaction between these two conditions. Is PTSD more than just one more consideration for veterans and their physicians to weigh in managing MS or does PTSD directly affect the course of the neurological disease?
Researchers at the VA’s Multiple Sclerosis Center of Excellence in Baltimore sought to better understand the impact of PTSD on their patients. “Psychiatric comorbidities in particular occur at rates in [patients with MS (PwMS)], either as a pre-existing condition or as a consequence of MS,” the researchers wrote in a study published in the Multiple Sclerosis Journal. “Current research has shown that both anxiety and depression can impact the disease course in MS.”1 Patients with MS who also have anxiety or depression are less likely to take their medications as prescribed, report greater fatigue and lower overall quality of life, and have a higher risk of suicide. Few studies have explored whether PTSD had a similar impact.1
A small study by the team found that patients diagnosed with PTSD before they received an MS diagnosis had a higher risk of clinical relapses and new brain lesions detected by magnetic resonance imaging (MRI).
To see whether this link was supported in a larger cohort, the researchers analyzed records from 96 veterans who had a PTSD diagnosis at least 30 days prior to being diagnosed with MS and 96 veterans with MS who did not have PTSD. Data was extracted from the VA’s Administrative Health Claims Database from the years 2010 to 2016 for individuals diagnosed on or before 2016 who also had at least two VA health care encounters between 2015 and 2019 in one of seven selected VISN regions. All veterans in the PTSD group had been found to have PTSD with service connection.
There were no significant difference in the two groups in terms of age, sex, race, demographics or clinical characteristics. The groups had comparable rates of depression and anxiety. Veterans in the PTSD group had a minimum rating of 30% for their disability. In addition, deployments were much more common in the PTSD group (60.2%) than in the control group (36.8%).
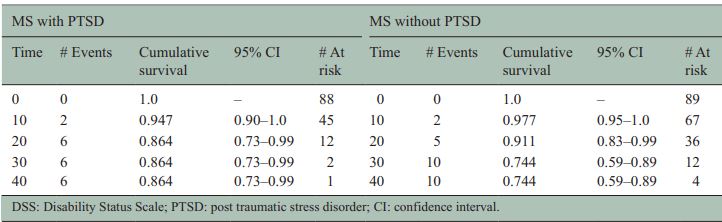
Click to Enlarge: Summary of Kaplan–Meier results for time to DSS 8 showing the number of events, cumulative survival, and number at risk at 10-year time intervals. Source: Multiple Sclerosis Journal
Higher Relapse Rates
Because of the small number of individuals with primary progressive MS (PPMS), statistical comparison were not performed for this type of MS.
Among those with relapsing-remitting MS (RMS), those in the PTSD group had significantly higher annual relapse rates (0.23 vs. 0.06, p=0.001) and number of new T2 lesions detected by MRI (0.52. vs. 0.16, p=0.007). The PTSD group also had higher rates of new gadolinium (GD)-enhancing lesions.
Veterans with MS and PTSD also experienced a much more rapid progression, reaching a Disability Status Score (DSS) of 6.0 at a mean of 23.7 years and median of 23 years and DSS 8.0 in 38 years (median 42 years). Patients without PTSD, in contrast, took a mean of 29.5 years and median of 30 years to reach DSS 6.0 and mean of 40.1 years and median of 46 years, though the team found the difference at DSS 8 to be not statistically significant.
They posited that the higher level of disease activity in the PTSD group could be related to an underlying neurochemical imbalance. “Both MS and PTSD individually have been implicated in abnormal regulation of neurotransmitters including dopamine, norepinephrine, epinephrine, neuropeptide Y, and serotonin,” the team noted. “In addition, inflammatory cytokines such as interleukin (IL)-1, tumor necrosis factor (TNF)-α, and interferon (IFN)-γ have been implicated in the role of depression in PwMS. Given that depression is very prevalent in MS and given neurochemical imbalance in both MS and PTSD, the synergy of both conditions could lead to greater clinical morbidity.”
They posited that the higher level of disease activity in the PTSD group could be related to an underlying neurochemical imbalance. “Both MS and PTSD individually have been implicated in abnormal regulation of neurotransmitters including dopamine, norepinephrine, epinephrine, neuropeptide Y, and serotonin,” the team noted. “In addition, inflammatory cytokines such as interleukin (IL)-1, tumor necrosis factor (TNF)-α, and interferon (IFN)-γ have been implicated in the role of depression in PwMS. Given that depression is very prevalent in MS and given neurochemical imbalance in both MS and PTSD, the synergy of both conditions could lead to greater clinical morbidity.”
The research supports previous findings. “Our results are not entirely unexpected in light of recent studies showing the association of PTSD and comorbid anxiety with increased activity in mS and the association of comorbid depression with greater disability progression,” the researchers wrote. Still, they noted, “while our morbidity outcomes in those with relapsing MS are novel, it would be important to replicate our findings in more diverse patient populations.”
The results could affect the clinical approach to patients with both MS and PTSD and the structure of the team treating these individuals. The researchers recommended multidisciplinary treatment teams to manage both physical and mental health concerns. Further, they noted that “because PTSD is a treatable condition, it would be of interest to design an intervention program targeting PTSD and related mental health disorders in PwMS to determine whether such a program would improve clinical outcomes.”
- Leekoff M, Culpepper W, Jin S, Lee-Wilk T, Wallin M. Impact of comorbid post-traumatic stress disorder on multiple sclerosis in military veterans: A population-based cohort study. Mult Scler. 2022 Jul;28(8):1257-1266. doi: 10.1177/13524585211058361. Epub 2021 Dec 2. PMID: 34854320.

