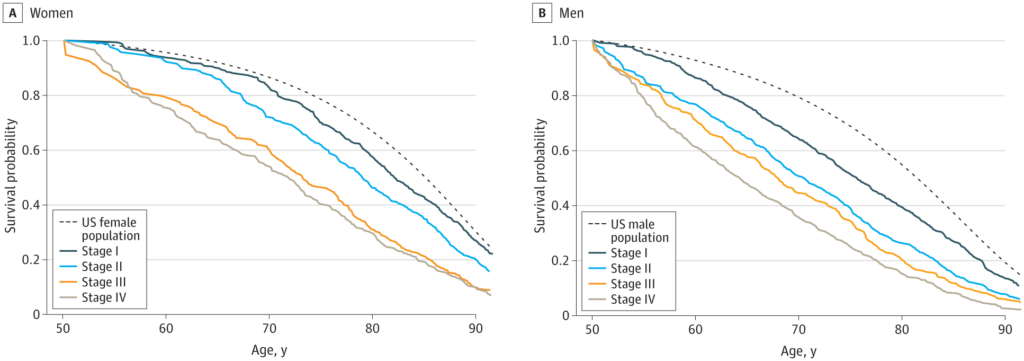
Click to Enlarge: Estimated Noncancer Survival Probability Among Patients With Oral Cancer Survival of patients with oral cancer given their own characteristics but as though they did not have oral cancer, compared with US 2011 life table estimates for female (panel A) and male (panel B) patients with oral cancer, conditional on surviving to age 50 years. Oral cancer patient data are from the Surveillance, Epidemiology, and End Results (SEER) Program, 2000-2011. Source: JAMA Network
WHITE RIVER JUNCTION, VT — Patients with oral cancer have a higher risk of death from noncancer causes compared to their counterparts of the same age and sex, and this risk increases by stage, according to a recent study.
The research published in JAMA Otolaryngology–Head & Neck Surgery evaluated how the competing risk of death from noncancer causes affects mortality rates from oral cancer. For the study, the researchers developed a new publicly available calculator, the Surveillance, Epidemiology, and End Results Oral Cancer Survival Calculator (SEER OCSC), which “provides personalized estimates of the likelihood of surviving or dying from oral cancer or other causes, for newly diagnosed patients ages 20 to 86 years,” the study reported.1
The study authors, including researchers from the White River Junction, VT, VAMC, sought to inform clinicians of the purpose of the SEER OCSC and provide a brief description of the tool.
Standard models for cancer prognosis “typically don’t include much specificity in characterizing competing illnesses or general health status when providing prognosis estimates,” according to the report, which added, “As a result, these models have limited usefulness for patients, “who must consider their cancer in the context of their overall health.” This is particularly the case for patients with oral cancer, who often have competing illnesses, the study explained, advising that the new calculator “provides personalized estimates of the probability of a patient surviving or dying from cancer or other causes, using oral cancer as the first data set.”
Eligible participants were between 20 and 94 years old with oral squamous cell carcinoma. The study used health data for 22,392 U.S. adults with confirmed oral cancer that came from the Surveillance Epidemiology and End Results (SEER) 18 registry, available SEER-Medicare linked data (by age of patient), the National Health Interview Survey with mortality follow-up, and U.S. lifetables.

Louise Davies, MD, MS, chief of otolaryngology-head and neck surgery at the White River Junction, VT, VAMC
“Our models showed that people with oral cancer have worse other-cause survival than the general population,” Louise Davies, MD, MS, chief of otolaryngology-head and neck surgery at the White River Junction, VT, VAMC, told U.S. Medicine. “They have a higher risk of death from noncancer causes than their age and sex-matched counterparts, and this is reflected in the calculator results. Even at localized stages, oral cancer patients have a higher risk of death from other causes than the U.S. population. As with other cancers, the risk of death from other causes rises at advanced cancer stages.”
For example, “given that a person has survived to age 50, a female and male diagnosed with stage III oral cancer would have a 60% and 44% chance respectively of being alive at age 70 in the absence of their cancer. In comparison, in the general U.S. population, the corresponding estimates are 86% and 79% respectively,” Davies explained in an email.
“This is an absolute difference of 26 and 35 percentage points respectively and shows us that this group has other competing illnesses that are affecting their life expectancy already, outside their cancer,” said Davies, who also is a professor at Geisel School of Medicine of Dartmouth College. “Our research did not specifically look at which noncancer causes of death might be greater or lesser in people with oral cancer compared to those who do not have oral cancer. However, oral cancer patients are particularly at risk of diseases such as COPD, liver disease and vascular disease, because the same things that put one at risk of getting oral cancer (alcohol and tobacco use) also cause these other competing illnesses.”
Patient age, coexisting illnesses, race, age, marital status, self-rated health status, place of residence and stage of tumor, which are all significant, were built into the model estimates. When people entered their data, these factors were included in the calculations that provide their health status adjusted age, life expectancy in the absence of cancer and chance of surviving, dying of the cancer or dying of other causes, Davies explained.
Higher Risk of Overall Death
The calculator showed that oral cancer patients have a higher than average risk of death from other causes than their matched U.S. population, and this risk increases by stage. In addition, this calculator is unique in treating the risk of death from other causes on equal footing with the consideration of the probability of death from the cancer, Davies added.
“Users of the system are provided with an estimate of the person’s health status-adjusted age, and the system uses those data to provide estimates of the likelihood that a person will survive, die of their cancer, or die of other causes,” she said. “These personalized estimates provide context for discussions about the place of cancer treatment in the affected person’s life as a whole. Something that has not been done before as far as we know. Particular values of the system are that 1) it provides numerical estimates that are representative of individuals in the United States, 2) the estimates reflect that there are competing risks of death operating simultaneously and 3) the estimated health status-adjusted age and the estimated life expectancy (in years) in the absence of cancer are modifiable.”
The researchers wanted to explore this topic because patients look for information about their prognosis when they are newly diagnosed with cancer, and clinicians also want data to help with advising patients. The National Cancer Institute’s Surveillance Epidemiology and End Results (SEER) Program publishes national population-based survival statistics annually that are helpful, but only in a general way, Davies explained.
“The estimates are not personalized,” Davies added. “They do not account for other illnesses a person might have that may also represent a threat to their life, and may in fact intervene either in conjunction with or before their cancer. I and my colleagues at NCI were interested in developing such a tool, and this is the first one that we developed, both developing and using new statistical techniques along the way.”
The study’s findings suggest that “survival estimates that exclude the effects of coexisting health conditions can lead to under or overestimates of survival,” Davies wrote.
“For this reason, we developed this tool to provide personalized data on life expectancy in the absence of cancer, and the tool also provides personalized estimates of the person’s chance of surviving or dying of their cancer informed by their overall health status, race, age, place of residence, sex and marital status,” Davies said, writing that the researchers want healthcare professionals to know this “tool is applicable to and will be useful for newly diagnosed patients with oral cancer and their clinicians.”
“Research shows that patients appreciate data that are personalized to them and many do want information on their prognosis,” Davies explained. “Among patients who helped in the development of this calculator, they said they appreciated knowing their prognosis not just for their cancer but overall. We recommend clinicians use the tool on their own as they think about their approach to a given patient but also consider using it together with their patients. We suggest they begin by asking patients what they want to know, as it varies by patient and may vary over time for the same patient. For patients who want prognosis information, being clear that these are estimates that don’t apply to a specific individual is important.”
“Furthermore, emphasizing that this is information that helps place things in perspective and encourages holistic thinking can also be helpful,” she continued. “People are more than their cancer diagnosis. Giving people the opportunity to consider their life as a whole is the aim of this tool. There are also links on the website for clinicians who would like to seek further guidance in communicating prognosis, which we recognize is a complex and important topic in providing high quality, sensitive care.”
In the future, the statistical methods developed for this first calculator, the use of two-time scales in competing risks modeling and the use of partially overlapping data sets will be applied next to other cancers and may also be helpful for other registry-based research. The system outputs are available in several different visual formats and can be printed out or saved, Davies said.
- Davies L, Hankey BF, Wang Z, Zou Z, Scott S, Lee M, Cho H, Feuer EJ. A New Personalized Oral Cancer Survival Calculator to Estimate Risk of Death From Both Oral Cancer and Other Causes. JAMA Otolaryngol Head Neck Surg. 2023 Jul 10:e231975. doi: 10.1001/jamaoto.2023.1975. Epub ahead of print. PMID: 37429022; PMCID: PMC10334297.
