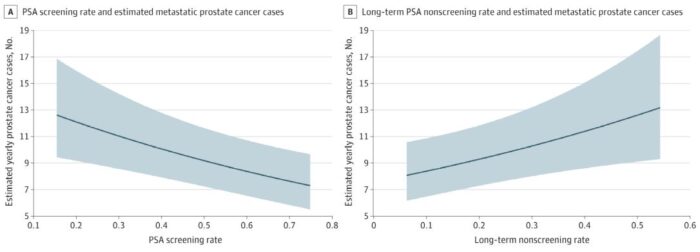
Click to Enlarge: Predicted case count estimates were generated from multivariable mixed-effects negative binomial models using a random effect of 0, continuous covariates at their mean values, Pacific region, and facility size of 40 889 men. Shaded areas indicate 95% CIs. Source: JAMA Oncology
ANN ARBOR, MI — Aside from skin cancer, prostate cancer is the most common cancer among male veterans. When diagnosed at an early stage, prostate cancer is highly curable. But even so, the benefits of screening with prostate-specific antigen (PSA) testing have been unclear.
The two largest randomized controlled trials of prostate cancer screening to date offered conflicting evidence on the risks and benefits of PSA testing. One suggested that PSA screening reduces risk of metastatic prostate cancer and prostate cancer death, while the other showed no benefit.
Over the past decade and a half, such conflicting data and corresponding changes in clinical practice guidelines have led to a decrease in rates of PSA screening nationally, followed by a rise in the incidence of metastatic prostatic cancer. While there is no direct epidemiologic evidence of a correlation between population PSA screening rates and subsequent metastatic prostate cancer rates, a large longitudinal VA study published recently in JAMA Oncology suggests that higher rates of PSA screening are, in fact, associated with lower rates of metastatic prostate cancer and vice versa.1
To better understand the role of PSA testing in a real-world setting and assess whether facility-level variation in PSA screening rates is associated with subsequent facility-level metastatic prostate cancer incidence, analyzed screening patterns and incidence of metastatic cancer for all men aged 40 and older with an encounter at 128 VA facilities from Jan. 1, 2005, to Dec. 31, 2019. At the study’s beginning, there were almost 4.7 million men in the cohort. By its end, the number had grown to over 5.3 million.
PSA Screening Decreased
Overall, the researchers found PSA screening rates decreased from 47.2% in 2005 to 37.0% in 2019, and the incidence of metastatic prostate cancer rose from 5.2 per 100,000 men in 2005 to 7.9 per 100,000 men in 2019.
Among the VA facilities, the researchers found a large degree of variability in screening rates, said lead author Alex K. Bryant, who is chief resident in the Department of Radiation Oncology at University of Michigan and the Ann Arbor, MI, VAMC.
“We then linked this variability in screening rates to facility-level rates of metastatic prostate cancer and found facilities with higher screening rates saw lower rates of metastatic prostate cancer and vice-versa,” he said.
This association was found for both yearly and long-term nonscreening rates. In facilities with lower yearly screening rates, for each 10% decrease in screening, there was a corresponding 10% increase in metastatic prostate cancer incidence five years later. For each 10% increase in long-term nonscreening rates, there was an increase of 11% in the incidence of metastatic prostate cancer.
“This result was robust in multiple sensitivity analysis, and after adjustment for potential confounders,” Bryant told U.S. Medicine. “While this is not a randomized trial, our study supports the idea that variation in PSA screening practices may be influencing real-world metastatic prostate cancer rates, and that increased screening could reduce the morbidity and mortality from metastatic prostate cancer—though this remains speculative given the observational nature of this study.”
Despite the conflicting findings concerning PSA screening in the literature, Bryant said he was not surprised by the new study’s findings. “I think the clinical trial data overall supports the idea that PSA screening reduces rates of metastatic prostate cancer, and, while it was interesting to confirm an association between screening and metastatic prostate cancer incidence in a real-world setting, these results were not surprising, given the clinical trial literature,” he said.
“The most important take-home message is that PSA screening may be influencing metastatic prostate cancer rates in the real world,” Bryant said. “This supports the idea that men who wish to maximally decrease their risk of metastatic prostate cancer should consider screening after discussion with their doctor.”
- Bryant AK, Lee KM, Alba PR, Murphy JD, et. al. Association of Prostate-Specific Antigen Screening Rates With Subsequent Metastatic Prostate Cancer Incidence at US Veterans Health Administration Facilities. JAMA Oncol. 2022 Oct 24:e224319. doi: 10.1001/jamaoncol.2022.4319. Epub ahead of print. PMID: 36279204; PMCID: PMC9593319.

