Older VA Patients Especially Resilient During COVID-19 Outbreak
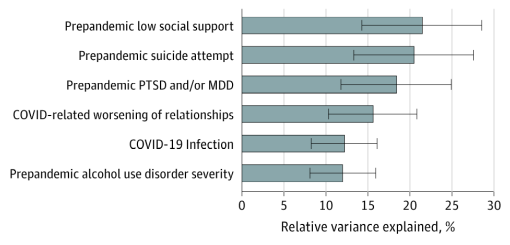
Click To Enlarge: Relative Importance of Significant Risk Factors and Correlates of New-Onset Suicide IdeationWhiskers indicate 95% CIs. MDD indicates major depressive disorder; PTSD, posttraumatic stress disorder.
SAN DIEGO — Past research has suggested that suicide rates rose during the 2018 influenza epidemic—unrelated to World War I and Prohibition—and during the 2003 severe acute respiratory syndrome outbreak among older adults in Hong Kong.
So, researchers thought it would stand to reason that the COVID-19 pandemic and the related illness, death and lockdowns, would drive suicide rates up, especially in older cohorts such as veterans. Interestingly, that does not appear to have occurred.
Authors of a recent study in JAMA Psychiatry noted that “prominent scholars have issued concerns that the COVID-19 pandemic may create a perfect storm for suicidality due to the unique juxtaposition of sustained social isolation and loneliness among at-risk individuals.– To this end, there have been recent calls to action to investigate longitudinal changes in and risk factors for suicidal behavior during the pandemic.”1
“Nearly a year into the pandemic, veterans as a whole showed great resilience in the face of the pandemic,” explained senior author Robert Pietrzak, PhD, MPH, director of the VA’s National Center for PTSD (NCPTSD NCPTSD’s Translational Psychiatric Epidemiology Laboratory, professor of psychiatry and public health at Yale University in New Haven, CT.
A study team led by researchers from the San Diego VAMC and the University of California, San Diego set out to determine the population-based burden of the COVID-19 pandemic on suicidal behavior among U.S. military veterans.
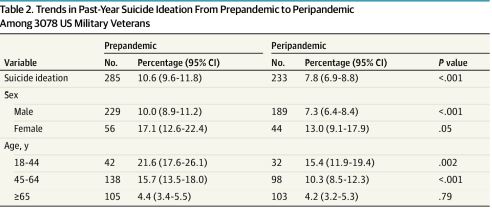
Click To Enlarge: Trends in Past-Year Suicide Ideation From Prepandemic to Peripandemic Among 3078 US Military Veterans
Researchers said they chose to focus on veterans because that appears to be “a population at disproportionately higher risk for suicidal behaviors during the pandemic,” they wrote, explaining, “First, older veterans were already at high risk for loneliness—which has been implicated as a robust correlate of SI and attempts—before the pandemic. Second, veterans have high rates of preexisting mental illness (e.g., post-traumatic stress disorder [PTSD], depression) and suicidal behavior relative to the general population, which may predispose them to deteriorations in mental health during the pandemic.”
The authors pointed to data collected before the pandemic, which indicated that the age- and sex-adjusted suicide rate among veterans had risen nearly 30% since 2010 and was at its highest recorded point in U.S. history. They also noted that, due to multiple chronic physical health conditions in many veterans, the cohort might have been especially anxious about deadly complications from COVID-19 infections.
Yet, after conducting the cohort study of 3,078 U.S. military veterans, rates of suicide ideation and suicide attempts did not appear to significantly increase from pre-pandemic levels during the pandemic at the population level. “However, a small proportion of veterans (2.6%) developed new-onset suicide ideation during the pandemic,” researchers advised.
“These results suggest that despite grim forecasts about the COVID-19 pandemic possibly creating a perfect storm for suicidal behavior, the prevalence of suicidality did not appear to increase among military veterans nearly 10 months into the pandemic,” the authors advised.
The population-based prospective cohort study used data from the first and second wave of the National Health and Resilience in Veterans Study, conducted from Nov. 18, 2019, to Dec. 19, 2020. Designated as median dates of data collection for the pre-pandemic and peri-pandemic assessments were Nov. 21, 2019, and Nov 14, 2020, which was almost 10 months after the start of the COVID-19 public health emergency in the United States.
The 3,078 veterans included in the study were aged from 22 to 99 years old, although the mean age was 63.2%. They were 91.6% men; with 79.3% non-Hispanic white veterans, 10.3% non-Hispanic Black veterans, and 6.0% Hispanic veterans included. Of those, 7.8% reported past-year suicide ideation, and 0.3% reported suicide attempts at the peri-pandemic assessment.
The study found that past-year SI decreased from 10.6% pre-pandemic (95% CI, 9.6%-11.8%) to 7.8% peri-pandemic (95% CI, 6.9%-8.8%).
On the other hand, 82 veterans (2.6%) developed new-onset SI over the follow-up period.
After adjusting for sociodemographic and military characteristics, researchers determined that the strongest risk factors and COVID-19-related variables for new-onset SI were:
- low social support (odds ratio [OR], 2.77; 95% CI, 1.46-5.28),
- suicide attempt history (OR, 6.31; 95% CI, 2.71-14.67),
- lifetime post-traumatic stress disorder and/or depression (OR, 2.25; 95% CI, 1.16-4.35),
- past-year alcohol use disorder severity (OR, 1.06; 95% CI, 1.01-1.12),
- COVID-19 infection (OR, 2.41; 95% CI, 1.41-5.01), and
- worsening of social relationships during the pandemic (OR, 1.47; 95% CI, 1.16-1.88).
“Veterans who reported a decrease in suicidal thoughts may have been better able to solicit social support during the pandemic by using virtual technologies,” suggested lead author Brandon Nichter, PhD, a clinical psychologist with the DoD and a visiting scholar at the University of California-San Diego.
Whatever the reason, the findings were somewhat unexpected, researchers conceded.
“The results of this cohort study suggest that, despite grim forecasts that the COVID-19 pandemic would exacerbate suicidality among U.S. military veterans, the rate of SI decreased at the population level nearly 10 months into the pandemic,” the authors concluded. “Veterans who were infected with COVID-19 were more than twice as likely to report SI, which suggests the need for future research to examine the potential link between COVID-19 infection and suicidal behavior.”
Profound Effects?
Background information in the study pointed out that the World Health Organization has warned that “the quarantining and social distancing measures enforced to reduce the spread of COVID-19—along with heightened financial hardship, unemployment, fear of contagion, and potential neurologic and psychiatric effects of COVID-19 infection—may have profound and long-lasting mental health effects.”
Indeed, in a population-based study published in February in JAMA Network Open widespread mental health consequences were identified in a representative sample of 5,470 U.S. civilian adults during the pandemic. Researchers, including representatives from the national Centers for Disease Control and Prevention and Women’s and Brigham Hospital in Boston, as well as international researchers, found that the prevalence of past 30-day suicide ideation (SI) increased slightly from 10.7% to 11.9% from June to September 2020.2
“Thus, in addition to the paucity of research examining trends in SI before and during the pandemic, a significant gap in the literature is that no prior studies have examined changes in more severe forms of suicidal behaviors, such as suicide attempts, which are stronger risk factors of suicide mortality,” wrote the authors of the veterans’ study. “Such data are vital to understanding the population-based burden of the COVID-19 pandemic on suicidal behavior, as well as for guiding intervention strategies and resource allocation.”
In the earlier research letter, overall, 1,710 (33.0%) reported anxiety or depression symptoms, 1,536 (29.6%) reported COVID-19–related trauma- and stressor-related disorder symptoms, 781 (15.1%) reported increased substance use, 618 (11.9%) reported having seriously considered trying to kill themselves in August, and 2,237 (43.1%) reported at least one of these symptoms.
Those researchers also determined that adverse mental or behavioral health symptoms were more prevalent among adults younger than 65 years vs. adults age 65 years or older (e.g., 18-24 years, aPR, 3.56 [95% CI, 3.04-4.18]) and among multigenerational caregivers vs. non-caregivers (aPR, 1.93 [95% CI, 1.78-2.08]) and respondents with prior psychiatric diagnoses vs. those with no prior diagnoses (aPR, 1.98 [95% CI, 1.83-2.15]).
Some of that was in line with what the veterans’ study found, according to the authors, who noted that veterans aged 65 and older had substantially lower rates of suicidal ideation both before and during the pandemic.
“Many older veterans have experienced multiple traumatic and stressful events, and may have been inoculated by these experiences to be better able to weather periods of prolonged stress,” Pietrzak said. “Having endured such events may have helped them develop adaptive coping strategies to better endure pandemic-related stress.”
- Nichter B, Hill ML, Na PJ, et al. Prevalence and Trends in Suicidal Behavior Among US Military Veterans During the COVID-19 Pandemic. JAMA Psychiatry. Published online August 25, 2021. doi:10.1001/jamapsychiatry.2021.2332
- Czeisler MÉ, Lane RI, Wiley JF, Czeisler CA, Howard ME, Rajaratnam SMW. Follow-up Survey of US Adult Reports of Mental Health, Substance Use, and Suicidal Ideation During the COVID-19 Pandemic, September 2020. JAMA Netw Open. 2021;4(2):e2037665. doi:10.1001/jamanetworkopen.2020.37665
