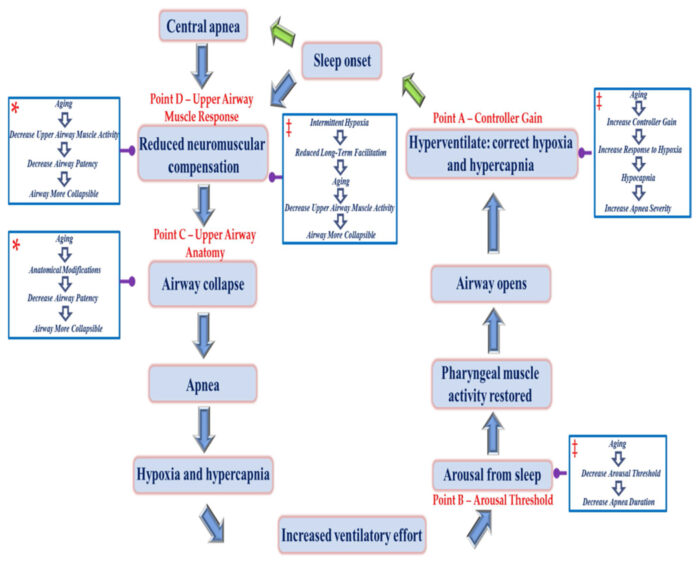
Click to Enlarge: Schematic diagram showing the sequence of events leading to the development of a central and/or obstructive apnea, and subsequent events that re-establish patency of the upper airway. Various points along the pathway (see points A–D) are highlighted. At each of these points, the mechanisms that contribute to sleep apnea (i.e., controller gain, arousal threshold, upper airway anatomy/collapsibility, and upper airway muscle responsiveness) are highlighted. In addition, the potential impact that aging in women (see boxes with blue outline and white fill) might have on the various mechanisms and ultimately the prevalence/severity of sleep apnea are highlighted. For example, aging in women could lead to upper airway anatomical modifications leading to increased collapsibility of the upper airway. Please note that the asterisk within the blue box indicates that there is published data which supports a link between age in women and the pathophysiological mechanism that impacts the prevalence and severity of sleep apnea. On the other hand, double dagger indicates that there is little evidence or no published evidence to indicate that these mechanisms are responsible for the increased prevalence of apnea in aging women.
Source: Curr Sleep Med Rep. 2021 Dec; 7(4): 177–185.
DETROIT — Obstructive sleep apnea, a disorder associated with persistent collapse or narrowing of the upper airway during sleep, has been linked to several detrimental outcomes including excessive daytime sleepiness, high blood pressure, neurocognitive decline and metabolic disorders.
Even though appropriately diagnosing and treating obstructive sleep apnea has important health implications, the condition in women is not well understood and likely to go undiagnosed, according to a recent study.
“Some standard metrics used to characterize sleep apnea, such as the apnea-hypopnea index [the number of apneas or hypopneas recorded during the study per hour of sleep] may not be indicative of the severity of the disorder in females,” explained Jason Mateika, PhD, a professor in the Department of Physiology at Wayne State University and VA Research Career Scientist at the Detroit VA Medical Center. “This is because some of the obstructive episodes experienced by women do not meet the formal definition of an apnea or hypopnea but nevertheless increase the work of breathing and ultimately, over time, may lead to cognitive dysfunction, fatigue, depression and insomnia because of fragmented sleep associated with these events.”
Mateika, along with postdoctoral researcher Qingchao Qiu, MD, PhD, authored a recent literature review that examines the pathophysiology of obstructive sleep apnea in aging women.
While the incidence of obstructive apnea increases with age in both women and men, women experience a sharp increase after menopause, they wrote. “Menopausal women tend to have a higher body mass index, neck circumference, and waist-to-hip ratio, along with higher fat deposition in the upper body and trunk area compared to pre-menopausal women. The modifications in visceral adiposity could provoke obstructive sleep apnea via excessive fat disposition in the parapharyngeal space, accompanied by an increased work of breathing.”
In the review published in Current Sleep Medicine Reports, Mateika and Qiu introduced four principal endotypes that contribute to sleep apnea: increased collapsibility of the upper airway (obstructive sleep apnea); a blunted upper airway muscle response to changes in the partial pressure of carbon dioxide (obstructive sleep apnea); a low arousal threshold; and instability of the ventilatory control system (i.e., increased loop gain). “These endotypes may be altered by many physiological variables, including sex and age,” they wrote. 1
Collapsible Airway
“In aging women, the increase in obstructive sleep apnea is linked to a more collapsible airway and reduced responsiveness of the upper airway muscles rather than the result of modifications to other variables (loop gain and arousal threshold) that can influence the severity of sleep apnea,” Matekia said.
He said the reduction in a phenomenon known as long-term facilitation of upper airway muscle activity—which is characterized by sustained increases in muscle activity—may contribute to the more collapsible airway in aging women.
Because the condition increases with age and affects women differently from men, a better understanding of the condition in aging women is important for VA clinicians, who are likely to see more cases of obstructive apnea in women as the female veteran population ages, Mateika said.
“VA clinicians should be aware of the signs and symptoms of obstructive sleep apnea, and the various options available for treatment of the disorder,” said Mateika. “Moreover, VA clinicians should be aware of how the signs and symptoms that are indicative of obstructive sleep apnea differ between men and women.”
“If we eventually get to a point where we are practicing precision medicine—that is, the exact mechanism responsible for the disorder is targeted—clinicians will need to understand that selected treatments for obstructive sleep apnea might vary based on sex and whether a female patient is pre- or post-menopausal.”
- Qiu Q, Mateika JH. Pathophysiology of Obstructive Sleep Apnea in Aging Women. Curr Sleep Med Rep. 2021 Dec;7(4):177-185. doi: 10.1007/s40675-021-00218-x. Epub 2021 Oct 3. PMID: 35211370; PMCID: PMC8865406.
