Survey Raises Questions of How Outside Care Could Meet That Need

“Camaraderie contributes to VA’s value proposition, and as care is increasingly provided in the community, finding ways to preserve camaraderie in both settings should be considered”.
McLEAN, VA — With all of the political debate about the increasing privatization of VA care—the Trump administration and many Republicans pushing it, while many Democrats are resisting—the voice of one important stakeholder group might be drowned out.
A new survey suggested that camaraderie (i.e., a desire to be around other veterans) is important to veterans who use the VA Health System.
The study was led by consultants Booz Allen Hamilton in McLean, VA, and also included participation from Stop Soldier Suicide in Durham, NC; Foundation Medicine in Boston; the National Center for PTSD at the White River Junction, VT, VAMC; the Geisel School of Medicine at Dartmouth in Hanover, NH; and the University of California Davis School of Medicine in Sacramento, CA.
The researchers surveyed 652 veterans to determine whether camaraderie is important to veterans who use the VA Healthcare System, especially for those veterans younger than 65 years old. Results were published in JAMA Network Open.1
“These findings suggest that camaraderie contributes to VA’s value proposition, and as care is increasingly provided in the community, finding ways to preserve camaraderie in both settings should be considered,” the authors wrote.
They added, “Unlike convenience, cost, and quality, camaraderie with other similar patients has not been reported as a prominent patient consideration when choosing a health care system or practitioner. As the Veterans Affairs (VA) Health System expands choice of practitioners for its enrollees, it is important to identify ways to promote veteran camaraderie in community care settings.”
In 2019, a web-based survey was administered to veterans who reported using VA healthcare. That survey included questions about cultural factors, such as camaraderie, practitioners’ understanding of veterans, trust of VA caregiver and a scenario-based question to ascertain whether veterans would choose VA or private healthcare if cost and distance were equivalent. Data analysis was performed from November 2024 to January 2025.
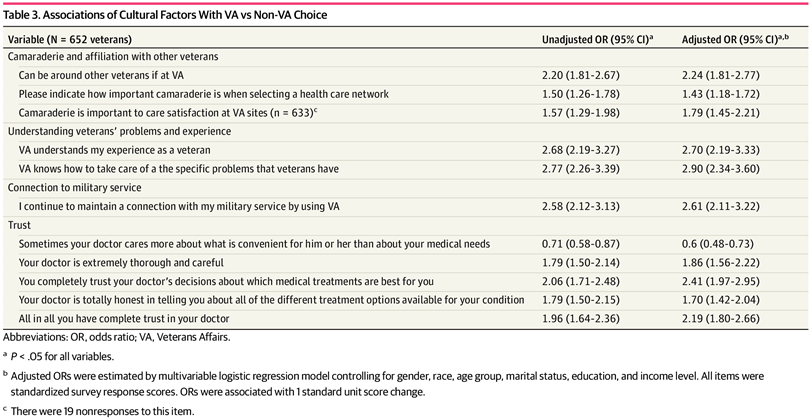
Click to Enlarge: Associations of Cultural Factors With VA vs Non-VA Choice Source: JAMA Network Open
Defined as the primary outcome was the importance of camaraderie in selecting a healthcare system or practitioner, measured as the percentage of veterans who reported positive ratings on relevant survey items.
Most of the veterans surveyed were male, 74.5. Respondents were categorized into three age groups: 18 to 34 years (246 veterans [37.73%]), 35 to 64 years (320 veterans [49.08%]) and 65 years and older (86 veterans [13.19%]).
Overall, 52.41% of respondents rated camaraderie and being around other veterans as important, with the percentage shooting up to 75.88% among veterans aged 18 to 34 years and to 65.35% for those aged 35 to 64 years.
Interestingly, only 35.75% of those 65 and older said they considered it important.
When asked whether they would choose VA or a private sector health system if cost and travel distance were equal, 69% of respondents indicated they would choose VA. The risk-adjusted model demonstrated that those who valued being around veterans were 2.24 times more likely (95% CI, 1.81-2.77) to choose VA.
“In this survey study of 652 veterans, camaraderie was important to most of these VA Health System users, especially younger veterans,” the authors pointed out. “As VA provides more choice of practitioners to its enrollees, it will be important to consider ways to preserve veterans’ ability to affiliate with other veterans in community care settings, especially for younger veterans who are often challenged in transitioning from military service to civilian life.”
“There are a number of reasons to believe that camaraderie is important to veterans,” according to the researchers. “Military unit cohesion is built upon a foundation of camaraderie (i.e., friendship, respect for and acceptance of individual differences, and mutual trust). Unit cohesion and camaraderie with peers are correlated with higher operational performance and lower risk of behavioral problems and posttraumatic stress disorder (PTSD) after military service.”
In addition, they pointed out, the transition from military service to civilian life can be challenging for many new veterans, explaining, that after leaving military service, “the camaraderie and cohesion associated with military social networks are ruptured. Alternative social networks have to be reactivated or developed, while simultaneously transitioning to a civilian culture.”
Exacerbating the challenges often are difficulties associated with employment, finances, housing insecurity and health issues. The study further advised that transition challenges are well known as contributors to substance abuse and suicide.
“Given the importance of camaraderie in the military and the importance of social support and peer relationships among veterans, we hypothesized that camaraderie and the desire to affiliate with other veterans are important to veterans who choose to use VA health care,” the study team stated. “This has not been previously documented and is typically omitted from discussions about the veteran health care experience and the value proposition of VA health care.”
First Study to Examine Issue
They said theirs was the first study to investigate the importance of camaraderie among patients and its role in the choice of healthcare system or practitioner.
While tradeoffs between convenience, cost and quality were important to the veterans surveyed—as they usually are with most consumers—the study noted that camaraderie also was a factor for those who had served in the military.
That camaraderie was especially important to young veterans wasn’t surprising, according to the researchers, “in so far as military experience and the culture, camaraderie, and social bonds associated with it are more recent for younger veterans. Accordingly, challenges associated with their transition to civilian life may cause them to place greater value on the social support from other veterans.
“In general, the importance of connection to military service was similar to the importance of camaraderie, both in its magnitude and in its importance to younger veterans,” they wrote. “It could be that certain organizational attributes and the iconography of VA sites create that connection, or it could be that the camaraderie experienced at VA is reminiscent of the camaraderie felt during military service, or both.”
The survey also found that veterans placed great value on VA’s ability to understand veterans’ experiences and specific problems, “which is an endorsement of VA practitioners’ cultural competency. This is reinforced by the wide range of specialized services VA offers to treat the health consequences of military service and war.”
Among those, according to the report, are expertise in prosthetics and rehabilitation; spinal cord injury; blindness rehabilitation; treatment of PTSD, traumatic brain injury, mental health disorders and suicide prevention; and treatment of toxic exposures.
The authors pointed out, however, that the “value of veteran social support, camaraderie, and military or veteran culture is typically not considered when weighing the benefits of the VA healthcare system. Our findings suggest that veterans value camaraderie and the ability to affiliate with other veterans, and that these factors contribute to their propensity to choose VA, especially younger veterans. With over 80 million outpatient visits each year, VA uniquely convenes large numbers of veterans at VA facilities. This creates opportunities for veterans to engage with each other, experience camaraderie, and sustain social relationships that may be beneficial.”
The 2018 MISSION Act provided veterans with enhanced choice of healthcare practitioners and, in fiscal year 2022, more than 40% of VA Health System enrollees received at least some of their healthcare by community practitioners.
While it might be difficult to create the same opportunities for veteran affiliation in the private sector, the authors suggested creating preferred provider networks of a select group of community practitioners who have demonstrated higher quality, greater cultural competency and a willingness to proactively share data with VA to enhance veteran care coordination.
“This may also enable some community-based practitioners to care for a sufficient volume of veterans so that they could create veteran outpatient environments or inpatient units that enable veteran affiliation and camaraderie,” they added. “VA’s existing partnerships with academic institutions could be the foundation for such a preferred network.”
- Vigilante K, Batten SV, Shang Q, et al. Camaraderie Among US Veterans and Their Preferences for Health Care Systems and Practitioners. JAMA Netw Open. 2025;8(4):e255253. doi:10.1001/jamanetworkopen.2025.5253


