VA Study Underscores Need for Viral Suppression
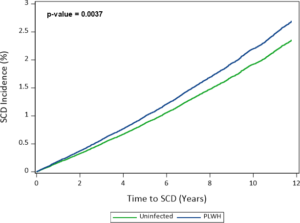
Click to Enlarge: Multivariable‐adjusted cumulative sudden cardiac death (SCD) incidence by HIV status.
Adjusted incidence output from a Cox proportional hazards regression model adjusted for age, sex, race/ethnicity, hypertension, diabetes mellitus, low‐ and high‐density lipoprotein cholesterol, triglycerides, hepatitis C infection, smoking status, renal disease, body mass index, anemia, cocaine dependence or abuse, alcohol dependence or abuse, chronic obstructive pulmonary disease, use of QT prolongation medications, and prevalent cardiovascular disease. PLWH indicates people living with HIV.
NASHVILLE, TN — A new veterans study underscored the critical need for viral suppression and heart disease risk factor modification among HIV patients. Researchers determined that those with sustained viremia or low CD4 cell counts had an excess risk of sudden death.
Vanderbilt University School of Medicine-led researchers emphasized that compliance with antiretroviral therapy as well as providing guideline‐based care for cardiovascular risk factors can be critical for those patients.
“People living with HIV are already known to have a higher risk of heart attack, stroke, heart failure, blood clots in the lungs and peripheral artery disease,” explained lead author Matthew S. Freiberg, MD, MSc, “We know that, among people with HIV, those who have a compromised immune system, for example a low total CD4+ T cell count, they seem to have a higher risk of cardiovascular disease than those who have high CD4+ T cell counts. It is unclear if a compromised immune system is a risk factor for sudden cardiac death.”
This study published in the Journal of the American Heart Association used data from the Veterans Aging Cohort Study, an observational, longitudinal cohort of veterans with and without HIV infection. Participants were matched 1:2 on age, sex, race/ethnicity and clinical site.1
Participants were followed from their first clinical visit on or after April 1, 2003, until the end of 2014. Researchers assessed whether HIV infection, CD4 cell counts, and/or HIV viral load were associated with World Health Organization (WHO)-defined SCD risk.
HIV patients made up 30% of the 144,336 participants; their mean age was 50, 97% were men (and 47% were of Black race. Researchers pointed out that, during follow‐up of about nine years, 3,035 SCDs occurred. They determined with that HIV infection was associated with increased SCD risk (hazard ratio [HR], 1.14; 95% CI, 1.04–1.25), adjusting for possible confounders.
“In analyses with time‐varying CD4 and HIV viral load, people living with HIV with CD4 counts <200 cells/mm3 (HR, 1.57; 95% CI, 1.28-–1.92) or viral load >500 copies/mL (HR, 1.70; 95% CI, 1.46-1.98) had increased SCD risk versus veterans without HIV. In contrast, people living with HIV who had CD4 cell counts >500 cells/mm3 (HR, 1.03; 95% CI, 0.90-1.18) or HIV viral load <500 copies/mL (HR, 0.97; 95% CI, 0.87-1.09) were not at increased SCD risk,” the study reported.
“HIV infection is associated with increased risk of WHO‐defined SCD among those with elevated HIV viral load or low CD4 cell counts,” the authors wrote.
Researchers adjusted age, sex, race/ethnicity, presence of heart or kidney disease, cocaine or alcohol dependence or abuse and various heart disease risk factors to find that the risk of sudden cardiac death was not increased in HIV patients who had healthy levels of infection-fighting CD4+ T cells or among those who had a low level of the HIV virus in their blood.
Progressively Higher Risk
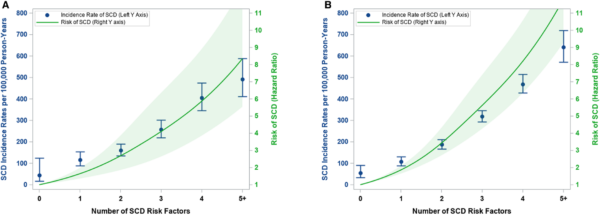
Click to Enlarge: Sudden cardiac death (SCD) risk among people living with HIV (PLWH) and veterans without HIV by number of SCD risk factors. A, Among PLWH and (B) among those without HIV. SCD risk factors: prevalent cardiovascular disease, hypertension, current smoking, hepatitis C infection, anemia, alcohol use disorder, chronic obstructive pulmonary disease. Incidence rates and hazard ratios (HRs) were adjusted for age, sex, race/ethnicity, CD4 cell count (PLWH only) and HIV viral load (PLWH only).
On the other hand, that risk was determined to be progressively higher with each risk factor for sudden cardiac death that was present. Those included existing cardiovascular disease, high blood pressure, smoking, hepatitis C infection, anemia, alcohol dependence or abuse and chronic obstructive pulmonary disease, regardless of whether they had HIV.
Still, the study reported that SCD was:
- 14% higher in people with HIV;
- 57% higher in people with HIV whose blood tests showed low levels of CD4+ T cells over time, an indicator that HIV was progressing and the immune system was compromised; and
- 70% higher in people with HIV whose blood tests showed that antiretroviral therapy had not suppressed the HIV viral load in their blood over time.
“Addressing risk factors related to both cardiovascular disease and HIV is essential to prevent the higher rates of sudden cardiac death in people with HIV,” said senior Zian H. Tseng, MD, MAS, of the University of California, San Francisco. “Clinicians should consider screening for specific warning signs of sudden cardiac death such as fainting or heart palpitations. And, if indicated, clinicians should request additional testing such as echocardiograms or continuous rhythm monitoring.”
The authors cautioned that results from the overwhelmingly male sample of study participants might not be generalizable to women. They also pointed out that HIV patients also had higher rates of myocardial fibrosis than those not infected, which could explain the higher rate of death due to lethal arrhythmias.
“In addition to HIV and cardiovascular risk factors, it is important for healthcare professionals to screen for and treat substance use disorders especially in people with HIV because they have a three times higher rate of overdose deaths presenting as cardiac arrest in our previous research,” Tseng said.
Background information in the article explained that people living with HIV (PLWH) have an increased risk of acute myocardial infarction, ischemic stroke, heart failure, pulmonary hypertension and peripheral artery disease compared with people without HIV.
“The mechanisms driving this excess risk of cardiovascular disease likely involve HIV‐specific factors including chronic immune activation and inflammation, antiretroviral therapy-related dyslipidemia, and behaviors such as smoking and alcohol consumption,” the researchers suggested. “These mechanisms and cardiovascular disease are also likely risk factors for sudden cardiac death (SCD).Whether HIV infection is an independent risk factor for SCD, however, is unclear because data are sparse.”
The objective of their study was to examine the association between HIV and SCD in a large national cohort of veterans with HIV and demographically and behaviorally similar veterans without HIV.
WHO criteria defines SCD as sudden unexpected death within one hour of symptom onset if witnessed or within 24 hours of being observed alive and symptom free (unwitnessed). This study used a four‐step process that included:
- review of each participant’s death certificate,
- review of administrative data from the VA and Centers for Medicare and Medicaid Services,
- manual review of clinical notes and data closest to the date of death that extended up to one year before the date of death within the VA electronic medical record, and
- review of non‐VA administrative data assessing whether participants were hospitalized outside the VA within one month of death.
- Freiberg MS, Duncan MS, Alcorn C, Chang CH, et. al. HIV Infection and the Risk of World Health Organization-Defined Sudden Cardiac Death. J Am Heart Assoc. 2021 Sep 8:e021268. doi: 10.1161/JAHA.121.021268. Epub ahead of print. PMID: 34493058.
- Matthew S. Freiberg, Meredith S. Duncan, Charles Alcorn, Chung‐Chou H. Chang, Suman Kundu, Asri Mumpuni, Emily K. Smith, Sarah Loch, Annie Bedigian, Eric Vittinghoff, Kaku So‐Armah, Priscilla Y. Hsue, Amy C. Justice, Zian H. Tseng. HIV Infection and the Risk of World Health Organization–Defined Sudden Cardiac Death: Journal of the American Heart Association. Sep 8, 2021. DOI: https://doi.org/10.1161/JAHA.121.021268
