15,000 Independent Pharmacies Initially Removed from Network
FALLS CHURCH, VA — The removal of about 15,000 independent pharmacies from the TRICARE network has created an uproar.
The military’s healthcare program announced in October that 15,000 community pharmacies not part of drugstore chains will no longer be in the TRICARE retail pharmacy network, adding in a press release that, “Even with the departure of these community pharmacies, the network will still offer access to more than 40,000 pharmacies.”
Express Scripts manages the TRICARE pharmacy retail network under a contract with the DoD. “The Defense Health Agency is confident that the new pharmacy contract maintains the quality of the TRICARE retail pharmacy network,” said Edward Norton Jr., chief of the Pharmacy Operations Division at the DHA. “Some independent pharmacies are leaving, but TRICARE families will continue to have access to an excellent network of pharmacies.”
Pharmacy groups adamantly disagreed. In a letter to U.S. Defense Secretary Lloyd Austin, the National Community Pharmacists Association (NCPA) said that eliminating the option for TRICARE beneficiaries to obtain their prescriptions at their pharmacy of choice should be reversed.
“The Department of Defense has awarded Cigna/Express Scripts a contract to continue administering the TRICARE pharmacy benefit and has allowed Cigna/Express Scripts to reduce the retail pharmacy network from 50,000 participating pharmacies to 35,000 pharmacies and to lower access standard thresholds creating additional obstacles for TRICARE patients,” wrote NCPA CEO B. Douglas Hoey, pharmacist, MBA. “They have done this despite the fact that of the 9.6 million TRICARE beneficiaries, 7 million of them use a retail network pharmacy each year. Unfortunately, this reduction has come at the expense of small-business independent community pharmacies and their TRICARE patients’ ability to access retail network pharmacies.”
Hoey also said it is unclear whether Express Scripts’ announcement in mid-November that the excluded pharmacies would be given another chance to join the network will make much of a difference because of issues about too low reimbursement.
“TRICARE patients earned their benefits, and it is imperative that they retain convenient access to their health care providers,” Hoey added. “With a vast majority of independent pharmacies out of the network, along with large chains such as Kroger and Walmart, it is difficult to see how Cigna/Express Scripts is meeting even the reduced access standards in its new contract with DOD. We therefore urge you to take steps to ensure all pharmacies that were included in the 2022 Tricare network remain in the 2023 network at the 2022 terms and conditions. Without this action, access to needed medications for TRICARE beneficiaries is in peril.”
The pharmacy network changes are estimated to affect about 400,000 TRICARE beneficiaries, with a disproportional impact on underserved rural and urban areas where most of the independent pharmacies are located.
Even worse, NCPA said, is that Express Scripts implemented the changes, effective Oct. 24, 2022, when pharmacies and beneficiaries expected the 2022 contract to last through the end of the year.
Legislators Complain
Legislators also expressed dismay at Express Scripts’ action. Sen. Jon Tester (D-MT), chairman of the Senate Committee on Veterans’ Affairs, demanded to know what the DoD is doing about the situation. “Our TRICARE beneficiaries deserve convenient access to the quality and timely benefits and care they have earned, and I will continue to strongly oppose any efforts to restrict that access,” Tester wrote in a letter to Undersecretary of Defense Gilbert Cisneros.
A letter from 100 bipartisan members of the House and Senate to Seileen Mullen, acting assistant secretary of defense for Health Affairs, asked the following questions:
- How is DHA monitoring current and future retail pharmacy participation in the TRICARE Pharmacy program?
- If future in-network pharmacy participation decreases, what steps will DHA take to ensure adequate access to in-person pharmacy services for TRICARE beneficiaries?
- Terminating the 2022 pharmacy contracts two months ahead of schedule will likely lead to a disruption of care for TRICARE beneficiaries. What reasons has Express Scripts given DHA for terminating the 2022 contracts early? Please outline what oversight DHA has over Express Scripts, as well as what authority DHA has given Express Scripts to make these contract changes.”
That effort was led by Sen. Tom Cotton (R-AR) and Rep. Buddy Carter (R-GA); Carter is a pharmacist.
Rep. Mike Johnson (R-LA) also sent a separate letter to Mullen, expressing concerns about how his beneficiaries in the areas surrounding Barksdale Air Force Base and Fort Polk in north Louisiana would be affected.
In announcing the change, Express Scripts pointed out that more than 90% of beneficiaries will have at least one network pharmacy within 15 minutes of their home. Those might be chain pharmacies, independent neighborhood pharmacies, grocery stores or wholesale warehouse stores, it said.
TRICARE beneficiaries who had a prescription at one of the pharmacies leaving the network were urged to take their medicine bottles to another participating network pharmacy, call their doctor’s office to have the prescription sent on to a new in-network pharmacy or call Express Scripts in-network pharmacy and ask them to transfer the prescription.
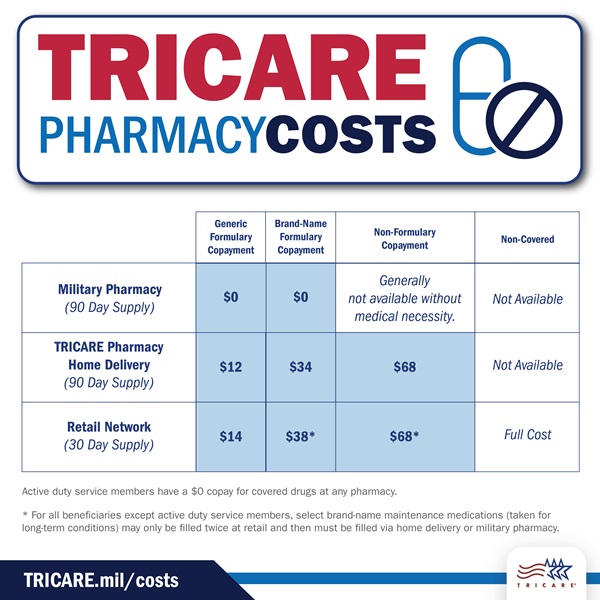
Beneficiaries also were cautioned about what will happen if they fill a prescription at a pharmacy that has left the TRICARE network. “As noted in the TRICARE Pharmacy Program Handbook, if you use a non-network pharmacy, you’ll pay full retail price for your medication. You’ll need to file a claim for reimbursement. Your claim will be subject to a deductible or out-of-network cost-shares and copayments,’ TRICARE advised.
In mid-November, Express Scripts said it would send a letter about a December contract solicitation directly to the pharmacies that either declined the recent contract or are affiliated with a wholesaler that declined the contract on their behalf. If the pharmacy accepts the contract, it would be able to rejoin the TRICARE network effective Jan. 15, 2023.
The NCPA said that many of the community pharmacies never even received the proposed contract for the 2023 retail network, which Express Scripts sent by fax. It also remained unclear whether any rates or terms will change in the new contracts being offered. More than 7,000 independent pharmacies accepted the proposed 2023 rates earlier this year.
“Cigna/Express Scripts offered contract terms to these independent pharmacies that were far below medication acquisition costs, forcing most independent community pharmacies to make the difficult choice to reject the terms, with no opportunity to renegotiate,” Hoey noted in his letter to Austin.