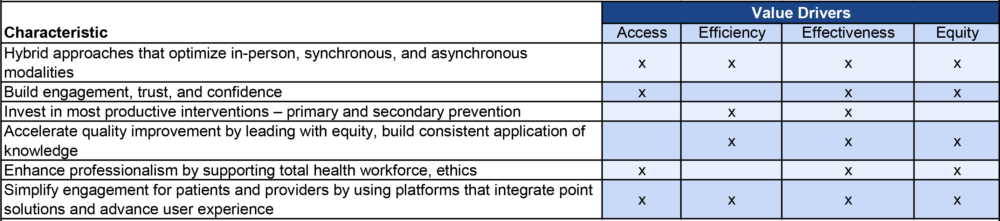
Click To Enlarge: Characteristics of a value-chain approach to digital health innovations. Source: Health Affairs Forefront
BOSTON — The VA introduced a new value-driven framework for evaluating health care innovations in conjunction with the Digital Medicine Society (DiMe) at the Healthcare Information and Management Systems Society (HIMSS) meeting in March. Unlike previous evaluation systems that have largely focused on financial savings, the VA/DiMe framework takes a holistic view of costs and benefits.
“We have an opportunity to redefine the blueprint for successful healthcare innovations. To be transformational, evaluation frameworks need to define true value as that which matters most to our veteran patients,” said VA Assistant Under Secretary for Health for Discovery, Education, and Affiliate Networks Carolyn Clancy, MD.
The VA defines value broadly in the new framework. In addition to point-in-time financial metrics, the system looks at quality of life, both population and individual-level benefits, and performance over time. It also weighs input from all stakeholders—veterans, providers, and administrators—to assess the effects of the innovation on patients and the health care system.
As both the country’s largest health care system and one that is free of pressure from third-party payers and investors to preferentially select healthy patients and keep costs low, regardless of the impact on care, the VA holds an unusual position in American health care. It is uniquely positioned to develop a comprehensive evaluation system for new devices and processes that have the potential to transform care and to scale up those that meet its standards on a national level.
“The VHA has an opportunity unlike any other, and we feel confident that this new evaluation framework will serve as a powerful reference for any decision maker in healthcare who is trying to make the right choices about the proliferation and innovation opportunities they face today,” said Jennifer Goldsack, CEO of DiMe. “DiMe is thrilled to partner with the VHA on this work, which has the potential to be successfully adopted by the rest of the healthcare market and initiate a new way of measuring success.”
The Need
The growth in digital applications for health exploded over the last two years as many patients, providers and health care systems switched away from in-person visits as a result of the pandemic. Even prior to the appearance of COVID-19, the VA had led the nation in building out telehealth services and implementing apps that enabled it to provide continuous care and specialist services to the nine million veterans in its care. With patients in all U.S. states and territories and a high percentage in rural or remote locations, digital health innovations have allowed the VA to reach—and stay in touch with—more veterans.
As a result, the agency had a jump on other health systems in the digital health field and a more sophisticated understanding of what works for a broad range of patients with complex needs. The VA understood the challenges and the benefits of digital care. As Clancy and her co-authors recently wrote in Health Affairs, “the digitization of health care is not a simple task; technologies should be implemented only if they will improve care for individuals and the systems that care for them. Thoughtful hybrid approaches will define digitization efforts, and humans—patients, care partners, communities, and clinicians—must be included in these endeavors. Human factors engineering is critical for all technologies, and even more so for health-related interventions.”1
Ideally, digital tools “democratize” health care, they wrote, meeting users where they are physically and culturally, with user-friendly interfaces, practical applications, and easy access at an affordable price point. On the flip side, the tsunami of data from digital innovations has the potential to overwhelm clinicians, lead to duplicative efforts, and flood the system with conflicting information that can make decision-making and coordination of care more challenging.
“To innovate the path to high value care, we must first redefine value beyond just dollars and cents. To ensure that every dollar invested returns value to the veterans we serve, we need to focus on measuring value across access, effectiveness, efficiency, and equity,” noted co-author Ryan Vega, MD, MHSA, chief officer, VA Office of Healthcare Innovation and Learning.
Developing the framework
To develop the framework, the VA team drew on more than 33 years of peer-reviewed publications on health care innovation and value framework, 80 evidence-based research publications, and interviews with more than 30 internal and external leaders.
The system includes fit-for-purpose value measures that include access, effectiveness, efficiency, and equity as measured by the ability to yield positive differences in a “way that matters to veterans and those who care for them.” The framework includes establishment of the appropriate scale and market to optimize value as well as recognition that “not all value measures may be achieved immediately, but rather may be realized over time” calculated in years.
The VA recommends three steps to deploying the framework. First, “demonstrate the balance of value being pursued across an innovation portfolio.” Then, use a holistic evaluation of the value promised by the innovations to determine appropriate investment. Finally, track the value returned from the portfolio with rigor.
Using the value-based framework, the VA introduced the PRIDE in all who served program, a 10-week health education program for LGBTIA+ veterans designed to reduce health disparities, 3D printing to provide patient-specific solutions, and the SmartHEART program, which has more than doubled participation in cardiac rehabilitation among veterans.
- Vega RJ, Goldsack JC, Patel S, Clancy C. Putting Digital Health Innovation into Practice: Learning from the VHA. Health Affairs Forefront. Feb 22, 2022. DOI: 10.1377/forefront.20220217.522347

