Performance Was Compared to Community Hospitals
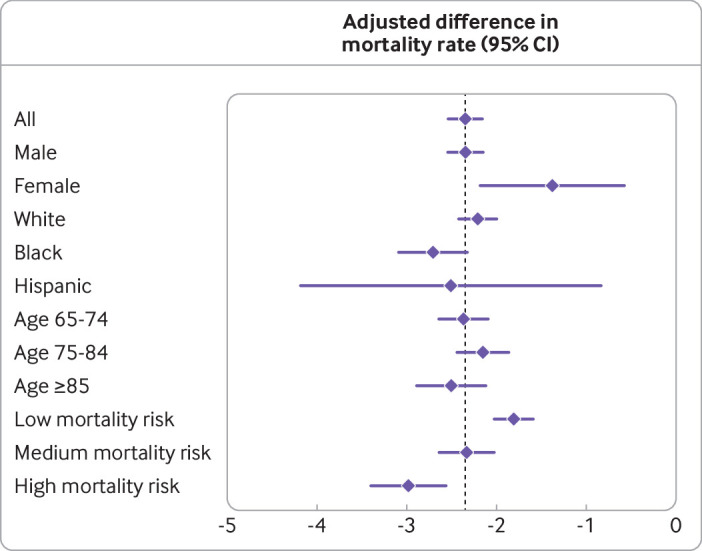
Click To Enlarge: Differences in adjusted 30 day mortality rates (in percentage points) between patients transported to Veterans Affairs hospitals and those transported to non-Veterans Affairs hospitals by ambulance, overall and by subgroups. Horizontal lines represent 95% confidence intervals. The vertical line shows the mean adjusted difference (–2.35 percentage points) in mortality rates for all patients in the study sample. Mortality rates were adjusted for patients’ residential zip code; level of life support available at destination hospital; type of location where ambulance ride originated; timing of ride (year, month, day of week); use of primary care, emergency care, and inpatient care in the prior year; sex, age, and race or ethnic origin; ICD-9 code (international classification of diseases, 9th revision; 1 digit) for in-ambulance diagnosis; and Elixhauser comorbidities. Table S3 provides details of these variables. Predicted mortality divided into three equal groups correspond to low, medium, and high risk categories. Table S6 provides details of the method, variables used to predict patient mortality, and regressions estimates in table form
STANFORD, CA — Long-standing concerns over the difficulties navigating VA’s large and complex healthcare system and the lack of choice veterans have about where to obtain their care have led to reforms in recent years that enable veterans to opt to obtain care in the private sector. The reforms are based, at least in part, on the premise that veterans are able to obtain quicker, and sometimes better, care outside the VHA.
A new study comparing mortality among veterans treated with emergency care at VA and non-VA hospitals is the latest in a growing number to suggest that the care received in VA hospitals compares favorably to that received in non-VA centers.1
The study, led by David Chan, MD, PhD, associate professor of Health Policy and investigator in the Department of Veteran Affairs at Stanford University, tracked mortality in a national cohort of 583,248 veterans aged 65 years or older who met two criteria: They were enrolled in both the Veterans Health Administration and the Medicare program and their care was initiated by an ambulance ride to obtain emergency treatment.
“Our findings indicate that within a month of being treated with emergency care at VA hospitals, dually eligible veterans had a substantially lower risk of death than those treated at non-VA hospitals,” Chan said in a press release issued by Carnegie Mellon University in Pittsburgh, which participated in the study. These veterans’ eligibility to receive care in both VA and non-VA hospitals, coupled with the emergency nature of their visit, reduced the potential for self-selection into one hospital type or the other, the study’s authors wrote. Most previous studies, on the other hand, were limited to comparing veterans receiving care in the VA healthcare system with non-veterans receiving care in non-VA settings and thus were unable to control for important underlying differences in the health status of veterans and non-veterans, according to the study.
The analysis, published in the BMJ, also accounted for other factors—for example, the ZIP code of the veteran’s residence, previous care patterns and the ambulance’s life-support capabilities—that might skew comparisons. The primary objective was to obtain a more balanced comparison of 30-day mortality risk after emergency care in VA vs. non-VA hospitals.
Of the cohort’s 1,470,157 ambulance rides (mean 2.52 rides per patient), 231,611 (15.8%) went to VA hospitals, and 1, 238, 546 (84.2%) went to non-VA hospitals.
Patients who went to VA hospitals had similar characteristics to those who went to non-VA hospitals, but with some noteworthy differences, the study found. For example, patients taken to VA hospitals were more likely to be Black and have used VA care in the prior year; they were also more likely to have mental health and substance use disorders.
In total, 9.32% of the patients taken to VA hospitals died within 30 days of their ride, compared with 11.76% of the patients taken to non-VA hospitals. The absolute difference of 2.35 deaths per 100 patients corresponds to a 20.1% lower mortality rate among patients taken to VA hospitals than among patients taken to non-VA hospitals.
The difference in adjusted mortality risk was similar for men and women. However, the mortality advantage associated with VA hospitals was particularly large for patients who were black -25.8%), were Hispanic (-22.7%), and had received care at the same hospital in the previous year.
Appropriate Care
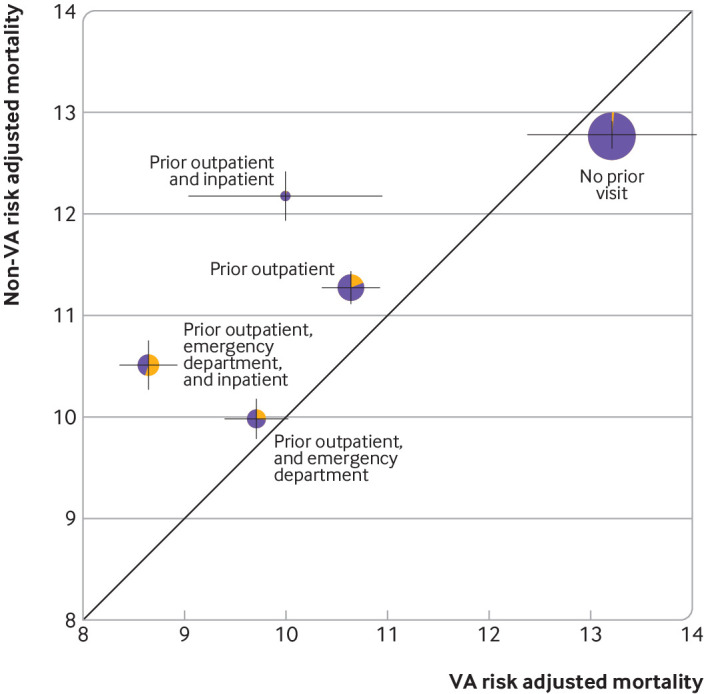
Click To Enlarge: Adjusted 30 day mortality rate (in percentage points) among patients transported to Veterans Affairs and non-Veterans Affairs hospitals by ambulance, by type of care received in the same hospital in the previous year. Bubbles indicate subgroups of patients receiving various types of care previously (outpatient, emergency, inpatient, or none). Figure shows five of a possible eight combinations of prior care that included more than 1000 ambulance rides to Veterans Affairs hospitals (fig S9 provides detailed estimates for all eight combination groups). Bubble areas are proportional to group size; shading shows the proportion of patients taken to Veterans Affairs hospitals (blue) and non-Veterans Affairs hospitals (red); bubble positions indicate adjusted mortality rate of groups (along x and y axes for patients transported to Veterans Affairs hospitals and to non-Veterans Affairs hospitals, respectively). Bubbles above and below the diagonal line indicate lower and higher mortality rates, respectively, among patients taken to Veterans Affairs hospitals than among non-Veterans Affairs hospitals (table S3 provides details of variables used to adjust mortality rates). To determine groups, an entity that shared the same Centers for Medicare and Medicaid Services certification number as a hospital that a patient visited in the prior year was defined as the same hospital. Table S7 provides details of the variables used for the regressions and regression estimates
Co-author David Card, PhD, professor of economics at the University of California, Berkeley, suggested that the perception that the VA health system falls short of providing appropriate care is generally incorrect, explaining, “findings suggest that, for the system overall, those perceptions do not match reality.”
While the study’s design allowed for a comparison of veterans to veterans, it also had some limitations, the authors noted. “Although our design mitigates the risk of confounding, it does not necessarily eliminate it. Systematic differences could still have existed between the patients taken to VA and non-VA hospitals and be associated with mortality risk,” the authors wrote. The authors also noted their results might not be generalizable to younger veterans or to episodes of care not initiated by emergency treatment. Further, the study was not designed to explain the mechanisms by which VA hospitals achieved lower mortality rates.
Nevertheless, the study’s findings have important implications for health policy, the authors stated. “Enabling or encouraging veterans to obtain care outside the VA system could lead to worse—not better—health outcomes, particularly for veterans with established care relationships at VA facilities,” they wrote, adding that the extent to which VA hospitals outperform other types of hospitals, and in what specific facets of care, should continue to be studied. “At the same time, increasing evidence of superior performance justifies a redoubling of efforts to understand how the VA system achieves this,” they wrote. “As well as helping the VA to improve care processes and outcomes, those insights could produce valuable lessons for healthcare delivery systems globally.”
- Chan DC, Danesh K, Costantini S, Card D, Taylor L, Studdert DM. Mortality among US veterans after emergency visits to Veterans Affairs and other hospitals: retrospective cohort study. BMJ. 2022 Feb 16;376:e068099. doi: 10.1136/bmj-2021-068099. PMID: 35173019; PMCID: PMC8848127.
- Chan, David C et al. “Mortality among US veterans after emergency visits to Veterans Affairs and other hospitals: retrospective cohort study.” BMJ (Clinical research ed.) vol. 376 e068099. 16 Feb. 2022, doi:10.1136/bmj-2021-068099
