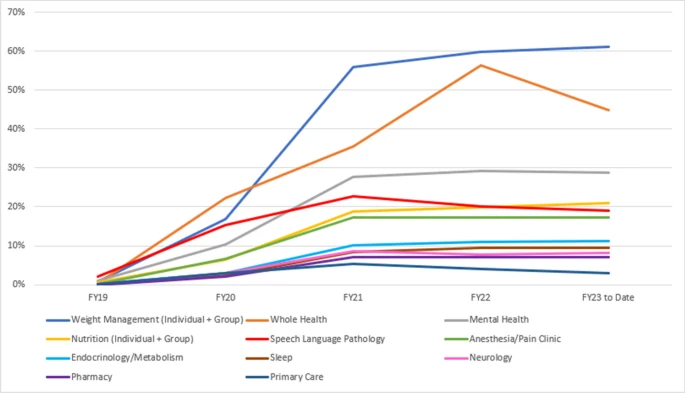
Click to Enlarge: Video-to-home encounters as a percentage of total encounters across all modalities among Primary Care and the top ten clinical specialties delivering video telehealth at VA, FY 2019–23. Source: Journal of General Internal Medicine
MENLO PARK, CA — Following the COVID-19 pandemic, telemedicine rates for veterans enrolled in VA healthcare services remained high, accounting for more than half of mental healthcare visits, while telephone-based care has decreased to pre-pandemic levels, according to a recent study.
The study, published in the journal Annals of Internal Medicine, analyzed trends in clinical outpatient encounters that took place in person, by telephone and by video for veterans receiving care at VA facilities before, during and after the COVID-19 pandemic.1
The study authors, affiliated with the VA Palo Alto Healthcare System in Menlo Park, CA and VA San Francisco Health Care System pursued this topic because of the “rapid expansion of telemedicine in the early days of the COVID-19 pandemic,” the authors explained.
“As clinicians and researchers evaluating the effectiveness and potential value of telemedicine, we realized the utilization of telemedicine was changing over time, and we wanted to understand how to account for patterns that were driven by the COVID-19 pandemic,” lead author Jacqueline M. Ferguson, PhD, a researcher at VA Palo Alto Health Care System, told U.S. Medicine.
The authors used data from electronic health records for patients within the VHA and identified more than 277 million clinical outpatient encounters through the VA’s Corporate Data Warehouse, which tracks data for nine million veterans enrolled in VA services. The encounters were categorized by care service (primary care, mental health and subspecialty care) and modality (in-person, telephone and video), the researchers pointed out.
The clinical outpatient encounters included in the study occurred between Jan. 1, 2019, and Aug. 31, 2023. The authors investigated several time periods: before the pandemic (before March 11, 2020), during the pandemic (March 11, 2020, through May 10, 2023) and after the pandemic (after May 11, 2023), defined by the end of the federal COVID-19 Public Health Emergency declaration, study authors explained.
On average, VA facilities had 1.14 million primary care, subspecialty or mental health encounters each week and 4.9 million encounters each month. Most VA patients are men (91%), 72% are white, and 65% live in urban areas, according to the study.
“We found telemedicine rates remain high following the COVID-19 pandemic, with more than half of mental healthcare visits being conducted remotely via video and phone,” Ferguson said. “While rates of telephone-based care have decreased to pre-pandemic levels, video-based visits have maintained at 11% of outpatient care, a notable 2,300% increase from pre-pandemic levels.”
“Our research suggests that telemedicine rates stabilized around May 2021—two years before the end of the federal COVID-19 Public Health Emergency declaration in May 2023,” Ferguson added.
Telemedicine has “gained popularity as a convenient way to receive care at VA, especially among mental health services, where video visits continue to increase,” Ferguson suggested. As of August 2023, telemedicine is used in 55% of all mental health visits (video: 35%, phone: 20%), 41% of all primary care visits (video: 4%, phone: 37%) and 21% of all subspecialty care (video: 4%, phone: 17%), Ferguson wrote in an email.
Changing Patterns of Use
“A key discovery in this study is the changing patterns of in-person and telemedicine use since the start of the pandemic,” Ferguson said. “Initially, high telemedicine numbers were due to limited in-person options. In the post-pandemic phase, which seems to start around May 2021, telephone-based care has largely returned to pre-pandemic levels, whereas video-based care accounts for 11% to 12% of outpatient care.”
“Notably, despite the reliance on in-person evaluations, about 10% of the in-person visits in primary care and subspecialty care have converted to telemedicine. This suggests that telemedicine will likely remain a popular way to receive care in the future, especially for mental health services, where 55% of care is now provided via telemedicine,” Ferguson added.
For healthcare professionals who are considering whether to offer telemedicine services to veteran patients, the authors suggest that “telemedicine visits have the potential to offer veterans convenient access to care by reducing travel burdens and associated costs.”
“This is especially valuable in the case of mental healthcare, where patients often have appointments as frequently as once a week,” Ferguson said. “For other types of conditions, telemedicine can sometimes act as a replacement or a complement to in-person care, depending on a patient’s specific needs. VA is continuing to study the effectiveness of telemedicine across a wide range of clinical services, which will hopefully generate evidence about how to optimally integrate telemedicine into clinical care.”
However, it’s important to note that “disparities in access to and use of telemedicine disproportionately affect older adults, individuals in rural regions and patients from historically marginalized groups,” the authors pointed out.
The study authors recommend that future studies “should consider evaluating quality, safety and health outcomes of telemedicine in this new equilibrium.”
Another recent article discussed 20 years of telehealth at the VHA. “Built with careful consideration over many years and tested during the pandemic, VA’s telehealth enterprise has proven to be robust, with approximately 40% of Veterans now receiving some kind of their VA care by telehealth,” according to the department’s Office of Connected Care/Telehealth. “VA, a health system with almost 30% of its patients living in rural or highly rural areas, was uniquely positioned to benefit from resource-sharing on a national level.”
The authors wrote in the Journal of General Internal Medicine, “As technology platforms evolved and proliferated and use cases matured, VA also began to grasp a range of related barriers—from the authority to provide care by telehealth and the infrastructure actually needed to optimize and maximize the delivery of telehealth services, to knowing how best to prepare veterans and their family members to use the technology.”
- Ferguson JM, Wray CM, Van Campen J, Zulman DM. A New Equilibrium for Telemedicine: Prevalence of In-Person, Video-Based, and Telephone-Based Care in the Veterans Health Administration, 2019-2023. Ann Intern Med. 2024 Jan 23. doi: 10.7326/M23-2644. Epub ahead of print. PMID: 38252945.
- Heyworth, L., Shah, N. & Galpin, K. 20 Years of Telehealth in the Veterans Health Administration: Taking Stock of Our Past and Charting Our Future. J Gen Intern Med (2024). https://doi.org/10.1007/s11606-024-08617-w

