LOS ANGELES — Amidst all the changes in therapies and protocols for treating stage I non-small cell lung cancer (NSCLC), the first step in treatment has remained the same for decades: surgery. The recommendations have been clear that any patient who can withstand surgery should have their tumor removed. Is it time to rethink the standard of care?
Researchers at the VA believe that it may be. They are conducting a potentially practice-changing study examining whether stereotactic radiotherapy should be considered an option in some patients who are fit for surgery. Stereotactic radiotherapy delivers very precise radiation to a tumor on an outpatient basis and has been used to slow progression of lung cancer in patients for whom surgery is not an option.
It may be a good option for elderly patients for whom surgery could be overly taxing, even though they technically meet the criteria for resection. As the average age for NSCLC diagnosis is about 70 years old, knowing whether radiotherapy provides better overall survival to some patients could have significant implications.
“This may be one of the most difficult and most important clinical trials in lung cancer,” said study co-chair Drew Moghanaki, MD, MPH, radiation oncologist at the Los Angeles VAMC and chief of thoracic oncology in the radiation oncology department at UCLA Health. “We feel that the data from this study will inform practice for many decades to come as new treatments continue to be discovered that can be combined with either surgery or radiation.”
The Veterans Affairs Lung Cancer Surgery Or Stereotactic Radiotherapy (VALOR) study, the largest study to ever compare the two treatments, has enrolled more than 200 of the anticipated 670 patients from participating VAMCs in Atlanta; Bay Pines, Fla.; Durham, N.C.; Hines, Illinois; Houston; Indianapolis; Long Beach, Calif.; Minneapolis; Pittsburgh; and Richmond, Va. As veterans are screened for lung cancer at these centers, they are offered the opportunity to participate in the study.
The U.S. Preventive Services Task Force recommends annual lung cancer screening for current or former smokers, who quit within the last 15 years, who are between the ages of 50 and 80 and have a 20 pack-year history of smoking. A pack year is defined as smoking one pack of cigarettes a day for one year.
Long-term Follow-up
The VALOR study aims to show which treatment for early stage NSCLC provides the best five-year survival rate, so final results will not be available for several years. A number of other studies, however, indicate that stereotactic body radiation therapy (SBRT) provides a good option for some patients and improves outcomes for those who go on to have surgery.
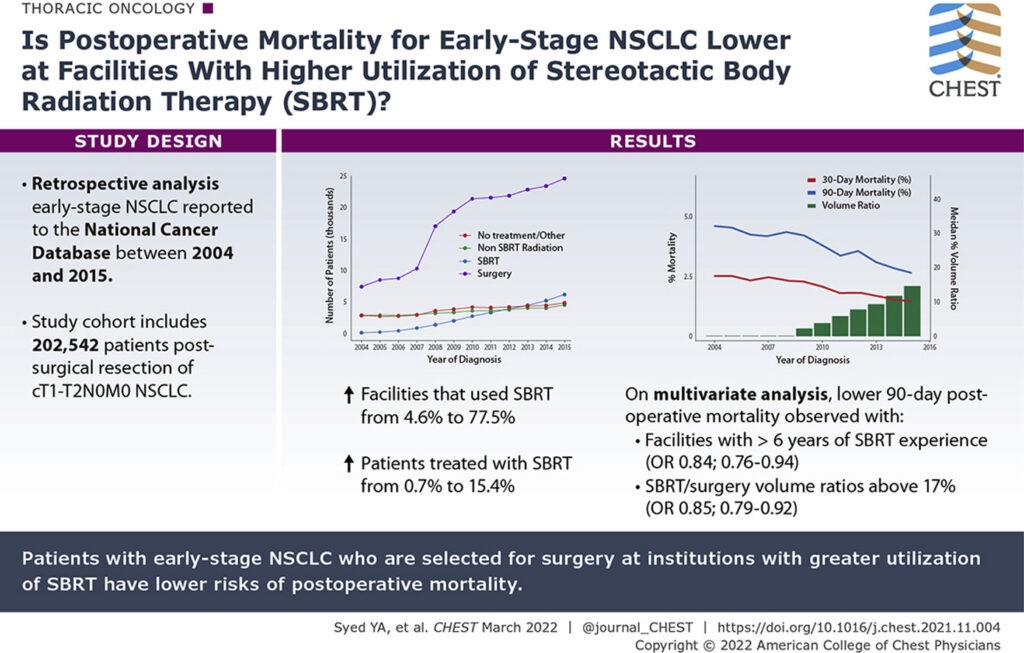
A recent study in Chest showed that patients who underwent resection at facilities with higher SBRT use had lower rates of postoperative morbidity. Researchers, including Moghanaki, analyzed data from 202,542 patients in the National Cancer Database with early-stage NSCLC from 2004 to 2015. They found that as the proportion of facilities that used SBRT increased from 4.6% to 77.5% and the proportion of patients treated with SBRT rose from 0.7% to 15.4%, the mortality rate for patients who had surgery dropped from 4.6% to 2.6%.1
The researchers concluded that “these findings suggest that the availability and use of SBRT may improve the selection of patients for surgery who are predicted to be at high risk of postoperative mortality.”
More specifically, “the availability of lung SBRT helps clinicians match the best treatment for each patient,” Moghanaki told U.S. Medicine.
Better Outcomes
Using the same database, another study published this fall in Clinical Lung Cancer found that “most early-stage NSCLC in the U.S. continues to be (appropriately) treated with upfront surgical resection,” Moghanaki said. “Their analysis also demonstrated that lung SBRT is being increasingly utilized as a treatment option for many who might otherwise be sent home to die without any treatment (often because they aren’t operable).”2
The percentage of all patients for whom observation rather than definitive treatment was the course of action halved between 2004 and 2017, dropping from 22% to 10.5%. Among Black patients, the change was even more stark, with observation plummeting from 32% to 15% as the proportion of Black patients receiving SBRT rose from 1% to 22%. That increase in SBRT increased the likelihood that Blacks would receive any curative therapy compared to white patients from 55% to 70% [OR: 0.55 (0.48-0.64) to 0.70 (0.62-0.79; P<.001].
In keeping with the findings seen in the Chest study, the Clinical Lung Cancer team reported that the “age-adjusted mortality rate of early-stage NSCLC decreased from 4.3 (4.0-4.5) in 2004 to 0.8 (0.7-0.9) in 2017 (P<.001).”
“These data provide national scale evidence through 2017 (>300,000 patients) about what can happen when patients have more treatment options than just surgery for early-stage NSCLC,” Moghanaki noted in a Twitter thread. He contrasted the results of this study with those found in a VA study from 2002 that determined that treating patients with SBRT only for symptomatic progression did not significantly improve survival compared to no treatment and that more than 50% of patients with early-stage lung cancer who did not receive definitive treatment died of the disease in less than two years.
“The introduction of lung SBRT continues to bend the survival curve for early-stage NSCLC,” Moghanaki said. “Let’s ensure this treatment is available at all hospitals; especially as the rise of early detection is helping us see more patients with early-stage NSCLC than ever before.”
Treating more NSCLC patients with SBRT will require a significant increase in access to the therapy. Moghanaki told U.S. Medicine that “about 75% of clinics in the U.S. appear to offer this treatment—which isn’t enough.”
- Syed YA, Stokes W, Rupji M, Liu Y, Khullar O, Sebastian N, Higgins K, Bradley JD, Curran WJ Jr, Ramalingam S, Taylor J, Sancheti M, Fernandez F, Moghanaki D. Surgical Outcomes for Early Stage Non-small Cell Lung Cancer at Facilities With Stereotactic Body Radiation Therapy Programs. Chest. 2022 Mar;161(3):833-844.
- Ganesh A, Korpics M, Pasquinelli M, Feldman L, Spiotto M, Koshy M. Increased Utilization of Stereotactic Body Radiotherapy is Associated with Decreased Disparities and Improved Survival for Early-Stage NSCLC. Clin Lung Cancer. Online 23 Sept 2022.