Vaccinations for Veterans, Servicemembers Half of Civilian Rate
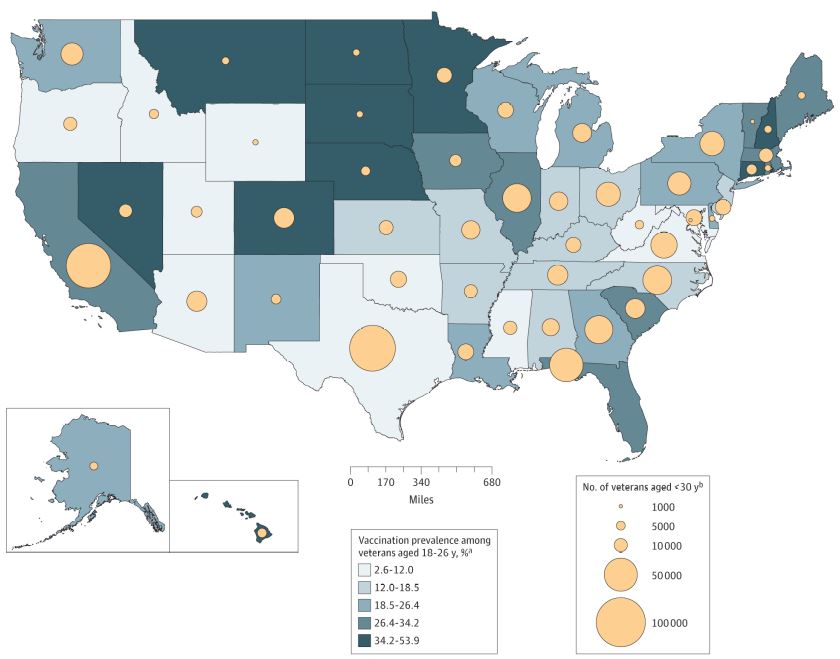
Click to Enlarge: Human Papillomavirus Vaccination Prevalence Among US Veterans Aged 18 to 26 Years and Number of Veterans Younger Than 30 Years by State
a. Data are from the Veterans Health Administration Corporate Data Warehouse
b. Data are from the US Department of Veterans Affairs Veteran Population Projection Model
Source: JAMA Oncology
ST. LOUIS—Eligible active-duty servicemembers and veterans have dramatically lower rates of human papillomavirus (HPV) vaccination, placing them at much greater risk of related cancers, according to a new study.
In fact, according to the research letter in JAMA Oncology, vaccination rates at the VA were half of the civilian rates. The vaccine is recommended for everyone under the age of 26.1
“Our findings should serve as a call to action to the Department of Defense and the Veterans Health Administration to advocate that their servicemembers get vaccinated,” said senior author José P. Zevallos, MD, chair of the Department of Otolaryngology at UPMC and the University of Pittsburgh School of Medicine. “Without intervention, these low HPV vaccination rates will lead to more HPV-associated cancers and deaths among future U.S. veterans.”
The study, with lead authors from Washington University School of Medicine and the St. Louis VAMC, included more than 128,000 veterans aged 18 to 26. It determined that only 30.2% of females and 18.7% of males had received HPV vaccination. That is compared to 62.4% of female and 37% of male civilians of the same age group who had been vaccinated.
HPV vaccination significantly lowers the risk of developing HPV-related cancers, which affect more than 45,000 people in the United States each year. Yet, according to the authors, no vaccination requirements or campaigns target the military/veteran population.
“Active-duty military service members and veterans are twice as likely as the general population to develop oncogenic HPV infections, resulting in a higher risk of HPV-associated cancers and mortality,” according to the report, “and HPV-associated oropharyngeal cancer, which occurs predominantly in males, is rising more rapidly among veterans than civilians.”
The study is the first to provide a national estimate of HPV vaccination prevalence among eligible veterans.
Using VHA data, researchers conducted a national cross-sectional study of veterans aged 18 to 26 years with at least one VHA primary care visit between Jan.1, 2018, and Dec. 31, 2020. They then constructed an age-matched representative sample of the U.S. population using the 2017 to 2020 National Health and Nutrition Examination Survey to compare HPV vaccination prevalence between civilians and veterans.
Included in the analysis were 128, 279 veterans (mean [SD] age, 24.4 [1.6] years; 79.2% males and 20.8% females). “Vaccination odds decreased with 1-unit increase in age (adjusted odds’ ratio [aOR], 0.95; 95% CI, 0.94-0.96) and increase in percentage of households living at 125% of poverty level or under (aOR, 0.83; 95% CI, 0.72-0.96),” the researchers pointed out.
The lowest vaccination rates were identified in Wyoming (6.1%; 95% CI, 3.1%-9.1%), Oklahoma (10.9%; 95% CI, 9.39%-12.41%) and Texas (11.9%; 95% CI, 11.35-12.45), while Hawaii (53.9%; 95% CI, 50.1-57.6%) and North Dakota (49.2%; 95% CI, 43.8%-54.6%) had the highest rates. The authors advised that Texas and Virginia were among states with the lowest rates and the largest populations of veterans younger than 30 years.
Zevallos suggested that, based on the findings, there needs to be “catch-up” HPV vaccination campaigns, especially in specific regions, to boost vaccination rates among veterans and reduce deaths from HPV-associated cancers. He pointed out that effective vaccination strategies could save the VHA millions of dollars in costs associated with treating largely preventable cancers.
“The VHA has spent approximately $136 million to treat HPV-associated cancers that are preventable with vaccination,” according to the report. “Without effective HPV vaccination strategies, the VHA will bear the financial burden of HPV-associated malignant neoplasms for decades to come.”
The research letter advised that high HPV-infection prevalence, rising HPV-associated oropharyngeal cancer incidence and low vaccination rates appeared to be associated with increases in HPV-associated cancer morbidity and mortality among veterans.
“The findings provide the VHA and Department of Defense an opportunity to design and implement HPV prevention campaigns, which could be extrapolated to civilians, among whom vaccination rates remain suboptimal,” the authors concluded. “In doing so, the VHA can prioritize cancer prevention and impart lessons to other health care delivery systems.”
- Chidambaram S, Chang S, Sandulache VC, Mazul AL, Zevallos JP. Human Papillomavirus Vaccination Prevalence and Disproportionate Cancer Burden Among US Veterans. JAMA Oncol. Published online, March 02, 2023. doi:10.1001/jamaoncol.2022.7944
