WASHINGTON, DC—As Vietnam-era veterans move into the age range in which most myeloproliferative neoplasms (MPNs) develop, the VA has a keen interest in fully understanding the full impact of exposure to Agent Orange in veterans with these malignancies.
The VA is particularly concerned with identifying any increased risk of cardiovascular disease associated with exposure to the dioxin-containing carcinogen in veterans with MPNs as heart failure, pulmonary hypertension and other cardiovascular diseases play a significant role in the morbidity and mortality associated with these hematological disorders.
MPNs include polycythemia vera, essential thrombocythemia, primary myelofibrosis and chronic myelogenous leukemia. The indolent course of most MPNs heightens the importance of long-term management of the disease and comorbidities.
Researchers from the Washington DC VAMC and colleagues sought to define the relationship between Agent Orange and CVD in veterans with MPNs to facilitate risk stratification and multidisciplinary management of patients. They presented their results at the 65th American Society of Hematology Annual Meeting on Dec. 10, 2023.1
They tapped the Veterans Affairs Informatics and Computing Infrastructure database to perform a case-controlled study from Jan. 1, 2006, to Jan. 26, 2023. They identified 93,269 veterans with three types of MPN (polycythemia vera, essential thrombocythemia and primary myelofibrosis) and matched them 1:1 by age, sex and race to veterans without MPNs from Illinois, which was chosen for its close representation of U.S. demographics. They then looked for composite CVD outcomes, including hypertension, hyperlipidemia, arterial thrombosis, venous thrombosis and bleeding.
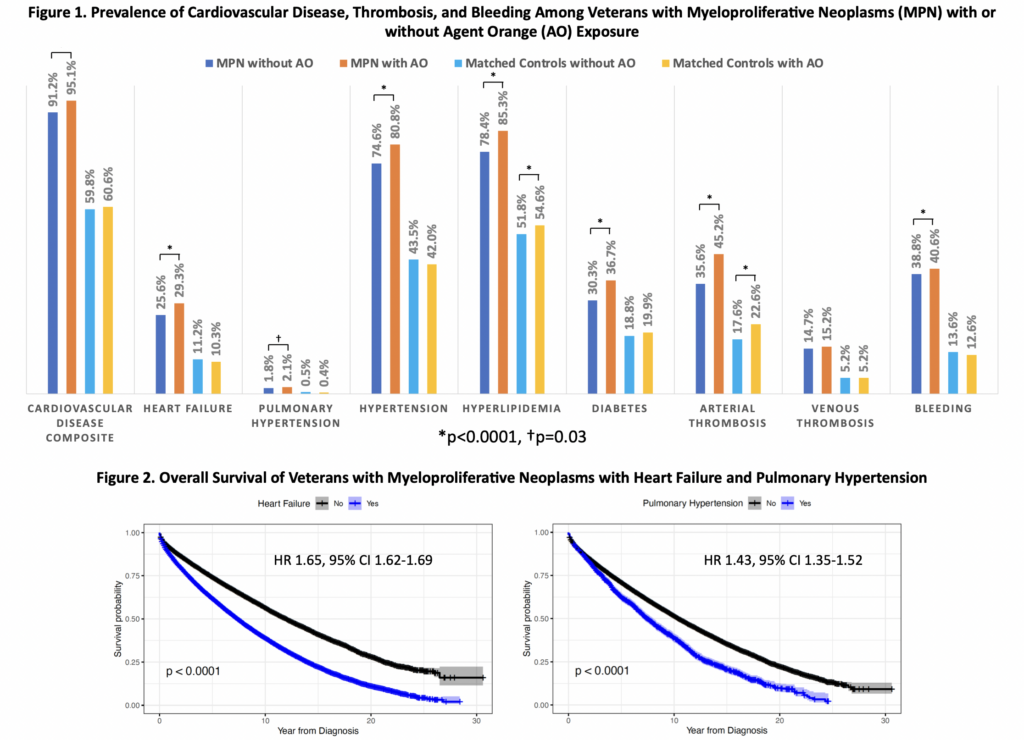
The team found that veterans with the three MPN subtypes examined had an increased prevalence of hypertension, hyperlipidemia, diabetes, heart failure and pulmonary hypertension. In addition, veterans with MPNs who had experienced arterial thrombosis, venous thrombosis and bleeding, had a significant association with heart failure and pulmonary hypertension (P<0.001).
Veterans with MPNs who also had Agent Orange exposure had higher rates of composite CVD and heart failure, pulmonary hypertension, arterial thrombosis and bleeding that those who had not been exposed to the herbicide.
Further, veterans born before 1960 who were exposed to Agent Orange had younger mean age of MPN diagnosis than those never exposed, 66 ± 7 (SD) years vs. 69 ± 10 (SD) years, p<0.0001, respectively. Veterans with MPNs with heart failure or pulmonary hypertension had lower overall survival than veterans with MPNs who did not have these comorbidities as well as controls.
“In summary, the CV risk factors, heart failure and pulmonary hypertension, are increased in veterans with MPNs and are associated with increased risk for arterial thrombosis, venous thrombosis, and bleeding complications,” the researchers concluded. “Not only is Agent Orange exposure associated with development of MPN, as previously reported, but Agent Orange exposure appears to increase CVD complications among veterans with MPNs.”
Source: Tiu A, McKinnell Z, Gill P, Antonio M, Shancer Z, Srinivasa N, Liu S, Diao G, Subrahmanyam R, Kessler C, Jain MR. Cardiovascular Outcomes Among Myeloproliferative Neoplasm Patients with or without Agent Orange Exposure Using a Large Veteran Database. Abstract 3202. ASH 2023. Dec. 10, 2023.
1Tiu A, McKinnell Z, Gill P, Antonio M, Shancer Z, Srinivasa N, Liu S, Diao G, Subrahmanyam R, Kessler C, Jain MR. Cardiovascular Outcomes Among Myeloproliferative Neoplasm Patients with or without Agent Orange Exposure Using a Large Veteran Database. Abstract 3202. ASH 2023. Dec. 10, 2023.


