SAN ANTONIO—Up to 40% of patients with diffuse large B-cell lymphoma (DLBCL) relapse or progress following first-line chemoimmunotherapy. Given the high rate of relapse, identifying the characteristics and outcomes associated with veterans with DLBCL who relapse could enable better monitoring or quicker intervention and potentially extend survival.
In an effort to define common features among those who relapse and increase understanding of disease progression among those who experience systemic, central nervous system (CNS) only or both types of relapse, investigators at the South Texas VAMC in San Antonio conducted a chart review of 6,266 veterans diagnosed with DLBCL between Jan. 1, 2011, and Dec. 31, 2021.
Supreet Kaur, MD, of the South Texas VAMC presented the study results at the 65th American Society of Hematology Annual Meeting on Dec. 11.1
Outcomes evaluated included response to first-line therapy, time to relapse and overall survival measured as the time between diagnosis and death. The team defined early relapse as stable or progressive disease as the best response to first-line therapy or disease progression within 12 months in patients who achieved complete or partial response.
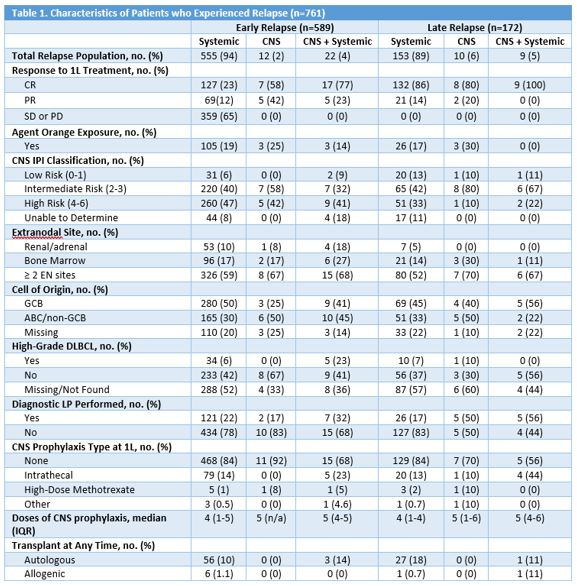
The study population was 97% male, and 65% had either stage II or stage IV disease; 90% had an ECOG performance status of 0-2. Three-quarters of the patients received a cyclophosphamide, vincristine, doxorubicin and prednisone (CHOP)-based regimen, and an equal number had an intermediate-or high-risk score on the CNS International Prognostic Index (CNS-IPI), a toll used to predict the risk of CNS relapse in patients with DLBCL.
With a median follow-up of 54 months, relapse occurred in 29% of veterans (761) with 27% experiencing systemic relapse, 1% CNS-only relapse and 1% both types of relapse. Among those who relapsed, 77% did so within 12 months, with a median time to relapse of 4.4 months. Among those who relapsed after one year, the median time to relapse was 25 months. No differences were detected in the characteristics of early versus late relapsers, though a higher percentage of those who relapsed early had a high-risk CNS-IPI score, bone marrow, renal or adrenal involvement.
Horowit AM, Nooruddin Z, Mader M, Franklin K, Williams M, Willams R, Blaize JP, Anath S, Song MM, Warnecke B, Pandya A, Djoumessi LRD, Lu L, Nazarewicz P, Espinoza-Gutarra S, Lucero KT, Whitehead J, Al-Abayechi A, Boyle L, Lee S, Souza GR, Naqvi M, Velez ET, Mines I, Kaur S. Differences in Characteristics and Outcomes of Central Nervous System Versus Systemic Relapse after First Line Therapy in DLBCL Patients: A Veterans Health Administration (VHA) Study. Abstract 5161. ASH 2023. Dec. 11, 2023.
Horowit AM, Nooruddin Z, Mader M, Franklin K, Williams M, Willams R, Blaize JP, Anath S, Song MM, Warnecke B, Pandya A, Djoumessi LRD, Lu L, Nazarewicz P, Espinoza-Gutarra S, Lucero KT, Whitehead J, Al-Abayechi A, Boyle L, Lee S, Souza GR, Naqvi M, Velez ET, Mines I, Kaur S. Differences in Characteristics and Outcomes of Central Nervous System Versus Systemic Relapse after First Line Therapy in DLBCL Patients: A Veterans Health Administration (VHA) Study. Abstract 5161. ASH 2023. Dec. 11, 2023.
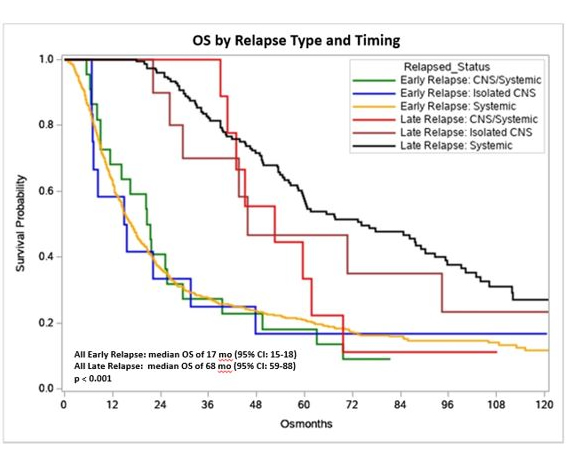
Across all three types of relapse, the median overall survival rate did not significantly differ, with the systemic group at 23.5 months (95% CI: 21-27), 30.6 months for the CNS-only group (95% CI: 15-71) and 29.6 months for the CNS plus systemic group (95% CI: 20-45), (p=0.75). Early relapse correlated with worse outcomes, regardless of type of relapse, with a median overall survival of 17 months (95% CI: 15-18). In contrast, patients with late relapse had a median overall survival of 68 months (95% CI: 59-88), (p<0.001).
The difference between the two groups can be seen vividly in the 24-month survival rates, only 37% for early relapsers and twice as high, 78%, for those who relapsed after 12 months. Among those who experienced late relapse, the veterans who had systemic-only relapses had the longest median overall survival, 74 months (95% CI: 60-90).
The researchers noted that previous studies suggested that certain features correlated with early or later relapse, but this study, the largest to look at outcomes for veterans with relapsed DLBCL, did not find any distinguishing features between those who relapsed early or later.
They drew attention to another finding of the study, instead, that the overall relapse rate and, specifically, the rates of CNS relapse were notably lower than previously reported. As a result, the use of CNS prophylaxis may not provide much benefit and might be reconsidered.
Given the poor outcomes for veterans who experienced early relapse, the researchers suggested that novel therapies such as chimeric antigen receptor T-cell therapy, might improve results.
1Horowit AM, Nooruddin Z, Mader M, Franklin K, Williams M, Willams R, Blaize JP, Anath S, Song MM, Warnecke B, Pandya A, Djoumessi LRD, Lu L, Nazarewicz P, Espinoza-Gutarra S, Lucero KT, Whitehead J, Al-Abayechi A, Boyle L, Lee S, Souza GR, Naqvi M, Velez ET, Mines I, Kaur S. Differences in Characteristics and Outcomes of Central Nervous System Versus Systemic Relapse after First Line Therapy in DLBCL Patients: A Veterans Health Administration (VHA) Study. Abstract 5161. ASH 2023. Dec. 11, 2023.


