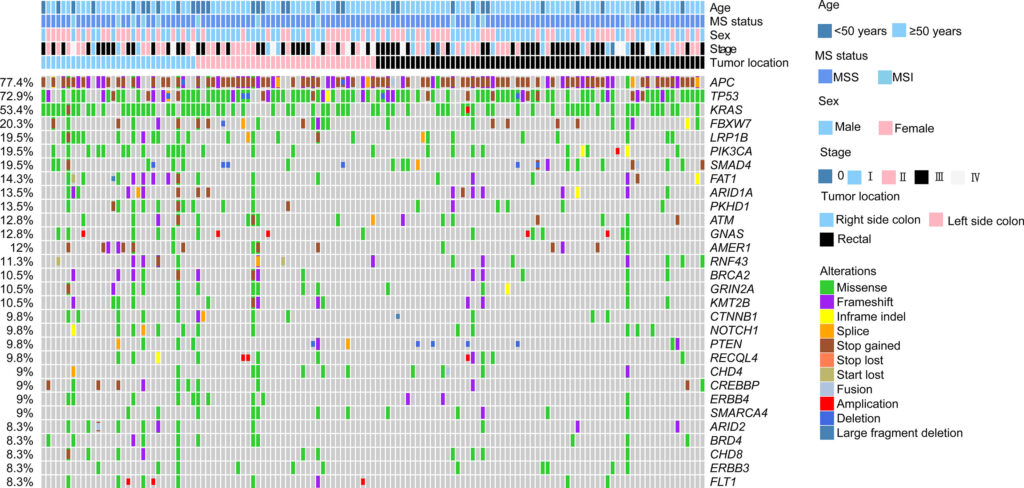
Click to Enlarge: Genomic landscape of colorectal cancer patients. The clinicopathological features including age, sex, stage, tumor location, and MS status were indicated by the bar on the top. The types of alterations were indicated by different colors. Each column represented one patient. Source: Frontiers in Oncology
HOUSTON — Patients receiving oncology care within a VHA facility are eligible for genomic- and other precision-testing, if they have an advanced-stage tumor or blood cancer and can tolerate recommended therapies.
That is an example of how VA, in some ways, has been cutting-edge in providing better care for veterans with advanced cancer. Others include partnering with the National Cancer Institute in an Interagency Group to Accelerate Trials Enrollment (NAVIGATE) to help patients gain access to clinic trials or joining with NCI and the DoD as part of the Applied Proteogenomics Organizational Learning and Outcomes network (APOLLO) to translate real-world data into better clinical care for veterans and active-duty servicemembers with cancer.
The issue is how available those opportunities are for veterans who need them. Nearly 30% of patients with MSI-H mCRC did not receive efficacious immune checkpoint inhibitors (ICIs), according to a recent study which also pointed out that, while disease-laterality data was not readily available, a substantial number of eligible patients also did not receive EGFR inhibitors.
“Colorectal cancer is the fourth most common cancer among veterans and the third leading cause of cancer-related death in the USA,” wrote the researchers led by the VA’s Center for Innovations in Quality Effectiveness and Safety in Houston and including Michael J. Kelley, MD, a professor at Duke University in Durham, NC, and the executive director of oncology within the VA. “Use of comprehensive genomic profiling (CGP) to guide administration of FDA-approved biomarker-directed therapies can improve outcomes among metastatic CRC (mCRC) patients.”
“As with other cancers treated by VA’s National Oncology Program, there are now several drugs that can be used to treat patients with metastatic CRC that are directed by results of molecular testing,” Kelley told U.S. Medicine. These include EGFR inhibitory antibodies (in RAS wild type), HER2 overexpression and immunotherapy (in MSI-high tumors). VA’s National Precision Oncology Program (NPOP) provides testing and consultation services that facilitate the use of precision oncology for veterans with CRC.
Kelley noted that NPOP also provides “access to [a] high sensitivity test, generally known as minimum residual disease, MRD, that can detect very small amounts of residual cancer after surgery. The use of this test for patients with stage II colon cancer can avoid the use of chemotherapy after surgery when the test does not detect cancer.”
The study authors sought to compute the rates of actionable biomarkers and prescriptions of associated FDA-approved therapies among veterans in NPOP. The findings were presented this past summer at the American Society of Clinical Oncology annual meeting in Chicago.
The study team queried the NPOP database to identify mCRC patients who had undergone comprehensive genomic profiling (CGP) via tissue or liquid biopsy between February 2019 and July 2022 and had one of the following five actionable biomarker profiles:
- NRAS/KRAS/BRAF wild type,
- BRAF V600E,
- MSI-H,
- TMB-H, or
- NTRK fusion or rearrangement.
At the same time, prescription rates for seven FDA-approved biomarker-directed therapies targeted agents and immune checkpoint inhibitors (ICIs) were extracted from VA’s Corporate Data Warehouse (CDW). The researchers assessed those prescription rates based on biomarker and patient characteristics, such as sex, race, ethnicity and rurality.
Results indicated that 908 mCRC patients underwent CGP, with 81.4% bearing colon adenocarcinoma (COAD) and 18.6% rectal adenocarcinoma (READ).
The authors reported that rates of actionable biomarkers associated with FDA-approved therapies were as follows:
- NRAS/KRAS/BRAF wild type (34.4%),
- TMB-H (9.6%),
- BRAF V600E (7.7%),
- MSI-H (5.6%),
- TMB-H and MSI-H (5.6%), and
- NTRK Fusion or rearrangement (0.3%).
The combined rates of any actionable variant were 47.4% for COAD and 44.4% for READ patients. Relative to patients without actionable biomarkers, patients with BRAF V600E mutations were more likely to be older and white; patients with NRAS/KRAS/BRAF wild type were more likely to be younger (all p < 0.001), according to the study.
Among the 424 eligible patients, the frequencies of FDA-approved CGP-directed therapy prescriptions were found to be:
- MSI-H (70.7%),
- TMB-H (47.4%),
- NRAS/KRAS/BRAF wild type (38.5%), and
- BRAF V600E (17.1%).
“Across all included biomarkers, African Americans (53.4%) were more likely to receive these therapies than whites (36.8%); and patients with prescriptions were more likely to be younger that those without (all p < 0.01),” the researchers pointed out.
The authors added that the underuse of EGFR inhibitors has been reported previously.
“There were racial and age differences in prescription rates,” according to the investigators, who urged further studies evaluating the barriers to prescribing CGP-directed therapies in the care of mCRC patients.
The age differences in germline genetic testing in younger colorectal cancer patients is especially concerning because of the increase in early onset cases, according to a recent article in the American Journal of Surgery.
University of Alabama at Birmingham researchers pointed out that young-onset colorectal cancer (YO-CRC) patients have high rates of pathologic genetic variants on germline testing but wrote that it remains unclear what factors are associated with genetic testing completion.
The study team performed a retrospective review of YO-CRC patients 50 and younger between 2014 and 2021; all participants received the entirety of their cancer care at a single institution. The primary outcome was defined as the completion of germline multigene panel testing, and variables were examined for association with germline multigene panel testing.
“Among 100 YO-CRC patients, only 31 % (n = 31) completed genetic testing,” the authors reported. “Testing rates did not differ by colorectal cancer stage but were significantly higher among patients who received chemotherapy (39.8 % vs. 5.9 %; p = 0.01) and in patients with increasing number of relatives with a family history of cancer (p < 0.01).”
The study concluded that only about one-third of YO-CRC patients completed genetic testing. “Patients seen by oncology or with increasingly strong family cancer history were more likely to complete genetic testing,” the researchers add.
- Djotsa AN, Winski D, Hoang-Anh Nguyen T, Ahmed S, et. al. Real-world rates of FDA-approved targeted therapy and immunotherapy prescriptions for patients with metastatic colorectal cancer in the VA’s National Precision Oncology Program (NPOP). Journal of Clinical Oncology. Volume 41, Number 16_suppl https://doi.org/10.1200/JCO.2023.41.16_suppl.3602
- Ficarino H, Cage B, Osula JP, Heatherly A, Chu D, Reddy S, Bhatia S, Hollis R. Deficiencies in germline genetic testing in young-onset colorectal cancer patients. Am J Surg. 2024 Jan 26:S0002-9610(24)00025-4. doi: 10.1016/j.amjsurg.2024.01.022. Epub ahead of print. PMID: 38302366.
