Smoking Makes Veterans Much More at Risk of Illnesses
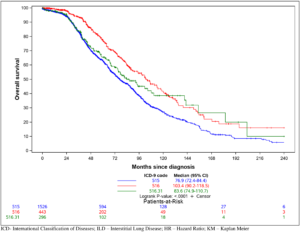
Kaplan Meier survival based on ICD-9 code.
Information obtained from electronic medical record review was used to define survival for all-cause mortality.
Interstitial lung diseases are a rare group of heterogeneous respiratory disorders which eventually lead to the development of fibrosis. With idiopathic pulmonary fibrosis being the most serious, veterans have substantially higher risks for ILDs, primarily because of high rates of smoking and history of smoking, according to a new review that calls for the VA to give the condition increased attention.
DURHAM, NC — Veterans are at a substantially higher risk for developing interstitial lung diseases (ILDs) than other cohorts, according to a new analysis which calls it “a critical issue.”
The study in PLOS One added that the findings call for “increased attention and awareness for ILD within the VA.”
A study team involving researchers from the Durham, NC, VAMC, Duke University and the University of North Carolina at Chapel Hill sought to describe the incidence/prevalence, clinical characteristics and outcomes of ILD patients within the VA’s Mid-Atlantic Health Care Network (VISN6).
To do that, the authors performed a multicenter retrospective cohort study of veterans receiving hospital or outpatient ILD care from Jan. 1, 2008, to Dec. 31, 2015, in six VISN6 facilities. Patients were identified by at least one visit encounter with a 515, 516 or other ILD ICD-9 code. Researchers noted that 3,293 subjects met the inclusion criteria, but 879 (26%) had no evidence of ILD following manual medical record review.
Results indicated that overall estimated prevalence in verified ILD subjects was 256 per 100,000 people with a mean incidence across the years of 70 per 100,000 person-years (0.07%). The prevalence and mean incidence specifically on patients with an ILD diagnostic code who had an HRCT scan or a bronchoscopic or surgical lung biopsy was 237 per 100,000 people (0.237%) and 63 per 100,000 person-years, respectively (0.063%), according to the report.
The authors also advised that the median survival was 76.9 months for 515 codes, 103.4 months for 516 codes and 83.6 months for 516.31.
A rare group of heterogeneous respiratory disorders characterized by progressive infiltration of the interstitium by immune cells and matrix producing fibroblasts, ILDs eventually lead to the development of fibrosis, according to background information in the article.
The most serious is idiopathic pulmonary fibrosis (IPF), which has a high association with substantial morbidity and mortality. For example, World Health Organization data of males diagnosed with IPF in the European Union (EU) defined the median mortality at 3.75 per 100,000 people in the EU from 2001-2013. In the United States, Medicare claims revealed that the total direct cost for patients with IPF was $26,000/person-year between 2001 and 2008, and the incremental cost over control subjects was $12,124.
“Despite the clear impact of ILD on human health and the ongoing efforts to define clinical characteristics, there remain considerable deficits in our understanding of the incidence and prevalence of ILD across various groups,” the authors wrote.
The VHA is the largest integrated health system in the U.S. and, within its database of more than 9 million subjects, includes many older males with smoking histories, which are known risk factors for increased ILD incidence.
“Based on this, it has been hypothesized that ILD is more prevalent in veterans’ populations. However, to our knowledge there have been no large epidemiological studies on ILD in veterans,” according to the researchers, who stated that their primary objective was to describe the incidence/prevalence, clinical characteristics and outcomes of patients with ILD who received care within that VISN.
Their focus was on six VHA medical facili ties and associated clinics in North Carolina—Asheville, Durham, Fayetteville, Salisbury—and two in Virginia—Richmond and Salem.
Subjects included had a median age of 69, with a wide age distribution. Most, 96%, were male, white, 79%, and current or former smokers, 75%. Their median BMI was 27.8, with 39% of the population considered overweight and 35% obese. The cohort also had numerous comorbidities, with airway disease being most common. Asthma was documented in 49%, overall, and COPD in 41%.
Researchers said it was consistent that 29% of the cohort had spirometric obstruction, although, “Interestingly, 65% of total cohort did not have pulmonary function testing recorded in the EMR.”
Another frequent comorbidity was gastroesophageal reflux disease in 40% of subjects. Lung cancer and mixed connective tissue disease were identified in 8% and 1%, respectively.
Nearly half, 47%, of the final cohort of about 2,400 had an ICD-9 515 code. While the ICD-9 groups were generally similar in terms of clinical characteristics 49% of 515 coded subjects had COPD vs. only 39% in the 516 grouping. Patients with no documented ILD on chart review had similar characteristics to those with ILD except for lower rates of smoking (29% never smokers) and COPD (30%), they added.
Risk Factors
“Our findings confirm the prevailing hypothesis that ILD is enriched within the VA. Though not proven in the present study, this is likely due to increased risk factors for ILD in veterans,” the researchers concluded. “Whereas the prevalence of ever-smoking is less than 50% among the general population in the U.S., we found smoking rates to be more than 70%, consistent with enriched smoking rates in veterans. Another potential explanation for the higher observed values is that our dataset evaluates a more generalized population than a specific registry. This is supported by recent studies using general population cohorts that demonstrated higher incident and prevalence rates than prior registry studies.”
The industry-funded study uncovered some anomalies, however. “Interestingly, we observed a difference in survival between the 515 vs. 516 groups, according to the report. “Generally, IPF is considered the ILD with the highest mortality risk. As IPF falls under the 516 group (coded as 516.31), we expected that 516 mortality would be worse than those coded as 515.” The authors generally attributed that to misclassification during coding and called for future studies to look at that.
The report also raised questions about the frequency of diagnostic testing and therapeutic interventions for ILD to determine how often veterans received appropriate interventions. It pointed out that The American Thoracic Society, European Respiratory Society and British Thoracic Society all provide best practice and guidelines on the diagnosis, treatment and monitoring of subjects with ILD. For example, high resolution computed tomography (HRCT) is considered critical for the initial diagnostic approach, and pulmonary function testing can help determine severity while serial pulmonary function tests have prognostic value.
“Despite relatively high performance of HRCT in this cohort, a significant proportion of the VA cohort did not receive PFTs, nor were these performed at later points as a measure to follow disease progression,” the authors wrote. “A possible explanation is that many veterans receive healthcare principally through community-based providers and are only infrequently followed at the VA. Therefore, some of these studies may have been performed outside the VA and were not captured in our database. Alternatively, it is possible that clinical care for ILD subjects in VA sites does not prioritize PFTs as an important clinical measure or that these patients have limited access to pulmonary providers with ILD expertise.
The study also cited low use of approved IPF therapies. While delays related to drug approval and central VA authorization were possible, “Alternatively, this could reflect an unmet need in the VA, particularly at VISN6 sites which are not affiliated with academic medical centers where there is access to ILD specialists. In future work, we plan to explore differences by facility and available site resources,” the researchers noted.
In addition to other limitations related to the specific VHA population and that veterans often receive care outside—as well as inside—the healthcare system, the study noted that “veteran deaths outside the VHA system are not generally recorded in the VHA data warehouse, thus potentially affecting our ability to accurately define mortality.”
Still, they said they succeeded in reporting the epidemiology of a large distinct cohort of VHA patients with interstitial lung disease “for the first time, to define the types and characteristics of ILD in a VHA population.”
- Article Source: Interstitial lung disease in a veterans affairs regional network; a retrospective cohort study
Bedoya A, Pleasants RA, Boggan JC, Seaman D, Reihman A, et al. (2021) Interstitial lung disease in a veterans affairs regional network; a retrospective cohort study. PLOS ONE 16(3): e0247316. https://doi.org/10.1371/journal.pone.0247316
