New Algorithm Helps Differentiate the Two Conditions
Nearly 70% of bipolar patients are initially misdiagnosed, and a third or more still haven’t gotten an appropriate diagnosis a decade later. Making the situation even more troubling is that many bipolar patients are being treated for major depressive disorder and receiving antidepressants alone – therapy that is suspected of actually destabilizing mood.
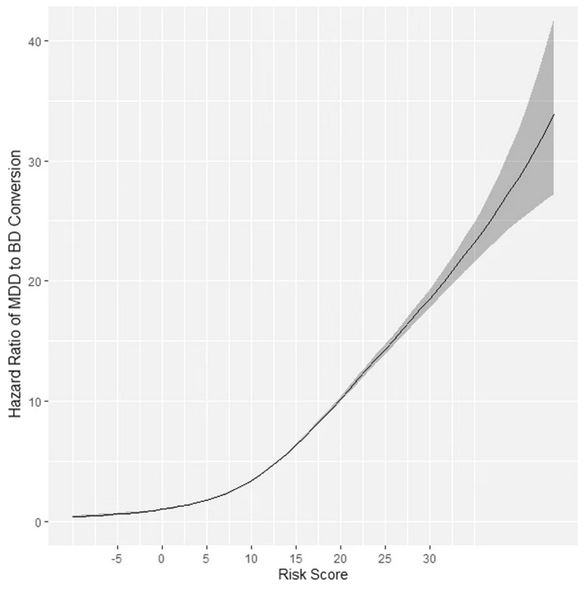
Click To Enlarge: The hazard ratio of diagnostic MDD to BD conversion as a function of risk score in the CCAE database. The gray “shadow” indicates the respective 95% confidence interval for the hazard ratio (y-axis). A risk score of 0 was used as a reference. MDD—major depressive disorder. BD – bipolar disorder. CCAE—IBM MarketScan Commercial Claims and Encounters database. Source: Transl Psychiatry 11, 642 (2021).
ALBUQUERQUE, NM — Misdiagnosis of bipolar disorder is extremely common. A survey by the National Depressive and Manic-Depressive Association earlier this century found that 69% of patients with the condition are misdiagnosed initially, and more than one-third remained misdiagnosed for 10 years or more.
The problem is not only that patients continue to suffer and fail to improve without proper treatment. Major depressive disorder is among the most common diagnosis, according to past research, and controversy rages over whether antidepressants alone are effective at all in treating bipolar depression and, even more fraught, whether they destabilize mood.
All of this has led to the phenomenon of patients transitioning from a diagnosis of major depression to bipolar disorder, often because of an initial misdiagnosis. A new study in Translational Psychiatry discussed the situation and offered a very practical tool: an algorithm that can predict a patient’s risk of transitioning from a diagnosis of major depression to a diagnosis of bipolar disorder.1
The effort, led by University of New Mexico Health Sciences Center researchers, also included participation from the Tennessee Valley VA Healthcare System and VA Informatics and Computing Infrastructure at the VA Salt Lake City Health Care System, as well as other U.S. and international institutions.
“Many patients with bipolar disorder (BD) are initially misdiagnosed with major depressive disorder (MDD) and are treated with antidepressants, whose potential iatrogenic effects are widely discussed,” the authors explained. “It is unknown whether MDD is a comorbidity of BD or its earlier stage, and no consensus exists on individual conversion predictors, delaying BD’s timely recognition and treatment.”
In response, the study team sought to create a predictive model of MDD to BD conversion and then validate it across a multinational network of patient databases using the standardization afforded by the Observational Medical Outcomes Partnership (OMOP) common data model.
To do that, researchers retrospectively analyzed five “training” U.S. databases: IBM MarketScan CCAE, MDCR, MDCD, Optum EHR and Optum Claims. In addition, external validation of the final prediction model was performed across nine patient record databases within the Observational Health Data Sciences and Informatics (OHDSI) network internationally.
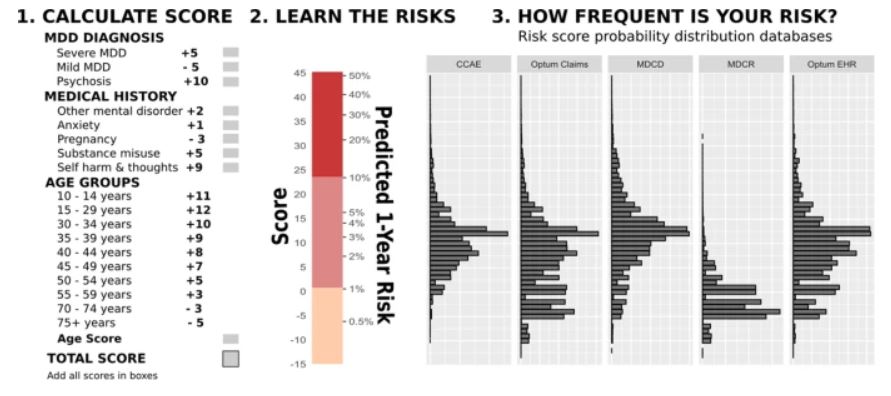
Click To Enlarge: The risk assessment algorithm for a one-year diagnostic transition from MDD (major depressive disorder) to BD (bipolar disorder).
CCAE—IBM MarketScan Commercial Claims and Encounters Database, MDCR—IBM MarketScan Medicare Supplemental Database, MDCD—IBM MarketScan Multi-State Medicaid Database, Optum EHR—Optum De-identified Electronic Health Record Dataset, Optum claims—Optum De-Identified Clinformatics Data Mart Database. “MDD diagnosis” scores are for depression severity and the presence of psychotic features within the index episode. “Medical history” events could occur at any time prior to and including the index visit. Source: Transl Psychiatry 11, 642 (2021).
The study reported that nine variables predicted one-year MDD-BD transition. Increasing the risk were:
- younger age,
- severe depression,
- psychosis,
- anxiety,
- substance misuse,
- self-harm thoughts/actions, and
- prior mental disorder.
“An assessment algorithm was built for MDD to BD conversion that allows distinguishing as much as 100-fold risk differences among patients and validates well across multiple international data sources,” the authors added.
Background information in the article advised that mood disorders are one of the three leading causes of disability worldwide. In the United States, more than 17 million people have been diagnosed with major depressive disorder (MDD) and seven million with bipolar disorder (BD).
Rates of serious mental illness appear to be especially high among servicemembers and veterans, at least partly because trauma exposure leads to various psychiatric disorders, including depression, anxiety, bipolar disorders, personality disorders and psychotic disorders. That is especially the case with post-traumatic stress disorder, according to a 2018 review.2
The issue is not limited to more recent veterans, however. At the VA, bipolar disorder affects large numbers of veterans across their entire life spans, with use of healthcare resources increasing over time. Older patients with bipolar disorder have unique treatment requirements and clinical presentations, according to the report in Psychiatric Services.3
The retrospective analysis of a large VA database was conducted by Case Western Reserve University School of Medicine researchers in Cleveland. It noted that, at the beginning of this century, the VA’s registry listed 65,556 patients as having bipolar disorder, with nearly one-fourth of them 60 or older and 10% 70 or older.
Is It an Earlier Stage?
“Both MDD and BD are chronic debilitating psychiatric conditions, with overlapping neurobiology and symptoms (recurrent depressive episodes), however, BD is diagnosed if at least one manic/hypomanic episode was present during the patient lifetime,” the Translational Psychiatry researchers pointed out. “It is debatable whether MDD represents an earlier stage of BD or is part of the same illness, given high MDD to BD prospective conversion rates (20-year rate of 25% and annual rate of 0.8-3.9%.”
They cited a retrospective study following up subjects with MDD for eight years; 7.6–12.1% of them subsequently had their MDD diagnosis changed to BD, with a mean time to change being 1.89-2.98 years.4
That matters because patients with BD have less favorable illness course, and outcomes require completely different treatments. “For example, antidepressants might trigger a manic mood switch among those with BD,’ according to the authors of the recent study. “It is suggested that the use of antidepressants by patients with unrecognized BD can contribute to their drug resistance, making them difficult to treat.”
On the other hand, a number of new drugs have recently gained Food and Drug Administration approval, including lumateperone, marketed as Caplyta, for treatment of adults with depressive episodes associated with bipolar I and II disorder, as monotherapy or adjunctive therapy with lithium or valproate and a combination of olanzapine and samidorphan, marketed as Lybalvi, which is approved for the treatment of adults with schizophrenia and for adults with bipolar I disorder, as a maintenance monotherapy or to treat acute manic or mixed episodes, as either monotherapy or an adjunct to lithium or valproate.
Lybalvi is especially notable, because it offers the effectiveness of olanzapine with less weight gain than schizophrenia, according to the FDA.
Previous research has suggested several factors that appeared to be predictive of MDD to BD conversion, but with inconsistent results. Those include younger patient age, treatment resistance, early depression onset, higher depression severity, multiple depressive episodes, family history of mood disorders, co-existing alcohol/substance abuse, attention-deficit/hyperactivity disorder, anxiety disorders, psychoses, suicide attempts, personality disorders, hospitalization, as well as rapid mood cycling, psychotherapy, living alone, prior use of psychotropic drugs and others. The authors explain that contradictory data also exist on the role of sex, age, depression onset and severity in MDD-BD transition.
The authors said their goal “was to develop a simple clinically useful risk assessment algorithm to help practitioners to recognize BD as early as possible among the patients presenting with MDD, and thus, to shorten the duration of untreated illness and mitigate the iatrogeny.”
The results, they pointed out, was “a simple, clinically understandable model for predicting one-year risk of diagnosis conversion from MDD to BD that validates well across multiple international data sources. Early onset of MDD, presence of psychotic features, severe depression, substance misuse and suicidality can serve as clinical predictors of prospective transition of a patient to BD diagnostic group and should get close attention from clinicians.”
Researchers also suggested that models extending beyond claims records and including physician notes and psychometric assessments could lead to more precise predictions of future conversions.
- Nestsiarovich A, Reps JM, Matheny ME, et al. Predictors of diagnostic transition from major depressive disorder to bipolar disorder: a retrospective observational network study. Transl Psychiatry. 2021;11(1):642. Published 2021 Dec 20. doi:10.1038/s41398-021-01760-6
- Compean E, Hamner M. Posttraumatic stress disorder with secondary psychotic features (PTSD-SP): Diagnostic and treatment challenges. Prog Neuropsychopharmacol Biol Psychiatry. 2019 Jan 10;88:265-275. doi: 10.1016/j.pnpbp.2018.08.001. Epub 2018 Aug 6. PMID: 30092241; PMCID: PMC6459196.
- Sajatovic M, Blow FC, Ignacio RV, Kales HC. Age-related modifiers of clinical presentation and health service use among veterans with bipolar disorder. Psychiatr Serv. 2004 Sep;55(9):1014-21. doi: 10.1176/appi.ps.55.9.1014. Erratum in: Psychiatr Serv. 2004 Dec;55(12):1442. PMID: 15345761.
- Li C-T, Bai Y-M, Huang Y-L, Chen Y-S, Chen T-J, Cheng J-Y, et al. Association between antidepressant resistance in unipolar depression and subsequent bipolar disorder: cohort study. Br J Psychiatry. 2012;200:45–51. doi: 10.1192/bjp.bp.110.086983.
