Authors of a new study strongly urged that patients with schizophrenia or schizoaffective disorder who have a history of suicide attempt and are younger than 59 or obese, should be monitored closely during the COVID-19 pandemic. They warned of the possibility of symptom exacerbation in those patients when they have severe COVID-19 since postmortem examination of brains in that cohort have revealed infection-related impaired brain neurotransmission.
HOUSTON — Schizophrenia patients have been especially hard hit during the COVID-19 pandemic, according to a recent study. Not only do they have a higher risk of contracting infection caused by the novel severe acute respiratory syndrome coronavirus 2—partly because they are less likely to be vaccinated—but also have a twofold increased risk of dying from COVID-19 compared to patients without mental illness.
The report in Complex Psychiatry pointed out that, even without a global pandemic, premature mortality is a well-known feature of schizophrenia, especially from suicide and comorbid somatic illnesses, most notably cardiovascular disease. Schizophrenia also is much more prevalent in the veteran population than nonveterans in the United States, explained researchers from the Michael E. DeBakey VAMC and colleagues.1
Past studies have estimated the prevalence of schizophrenia from 1.4% in a general veteran sample to 11.2% in older adult veterans; that is compared to a range between 0.25% and 0.64% in the overall U.S. population, according to the article.
“There is, therefore, a need to identify vulnerability factors for COVID-19 in patients with schizophrenia which can guide the allocation of preventative and therapeutic resources and reduce mortality in this patient population,” the authors wrote.
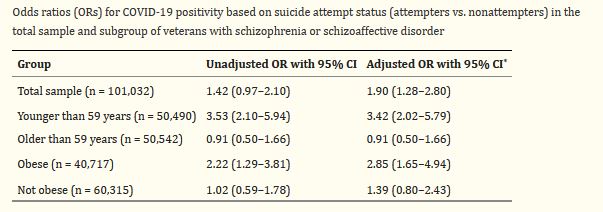
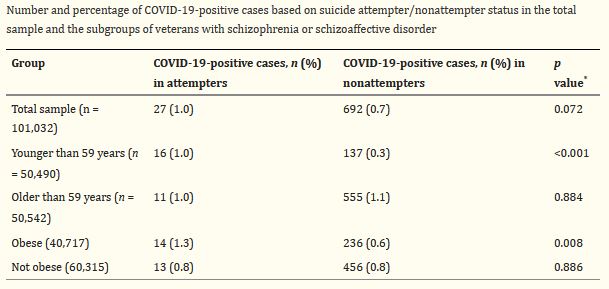
Click To Enlarge: *Adjusted for age, sex, race, marital status, BMI, and total Charlson-Deyo score. Source: Complex Psychiatry. 2021 Dec 1; 392: 1789–1795.
To achieve that, the study team conducted a cross-sectional analyses of electronic health records of veterans with a diagnosis of schizophrenia or schizoaffective disorder that received treatment at any VAMC between Jan. 1, 2020, and Jan.31, 2021. Included in the analyses were 101,032 veterans with a mean age of 56.7, and 90.8% of them were males.
During that time period, 2,703 (2.7%) of the patients attempted suicide, and 719 (0.7%) patients were positive for COVID-19. Researchers determined that the association between history of suicide attempt and COVID-19 positivity was affected by age and BMI, so that the relationship was only significant in patients younger than 59 years and in obese (BMI ≥30) patients (adjusted OR 3.42, 95% CI 2.02-5.79 and OR 2.85, 95% CI 1.65-4.94, respectively).
“Higher rates of COVID-19 in young or obese suicide attempters with a diagnosis of schizophrenia or schizoaffective disorder might be due to the elevated risk for the infection in this subgroup of patients,” the authors concluded.
Researchers added that, to their knowledge, this was the first study to identify a link between history of suicide attempt and COVID-19 in veterans with schizophrenia or schizoaffective disorder.
“The association of history of suicide attempt with COVID-19 in veterans with schizophrenia or schizoaffective disorder may be explained by psychological factors which both predispose patients to suicide attempts and make them more vulnerable to COVID-19 infection,” they explained. “For example, anhedonia, impulsivity and substance use are associated with suicidal behavior and have also been associated with less likelihood of adopting COVID-19 precautionary behaviors such as physical distancing, wearing a mask, or handwashing.”
The authors suggested that the association of history of suicide attempts with COVID-19 positivity in the younger and obese subgroups also is worth more discussion. “For example, suicide risk in schizophrenia is highest for young adults but lowest for patients older than 65 years, and although BMI has not been associated with suicide risk in schizophrenia or schizoaffective disorder, obesity is associated with higher levels of immune system dysregulation and inflammation in patients with schizophrenia. Relatedly, markers of immune dysregulation and inflammation in the periphery and central nervous system are elevated in suicide attempters relative to nonattempters,” they noted.
The researchers also pointed to recent research associating primary humoral immunodeficiencies with psychiatric disorders (including schizophrenia) and suicide attempts in the same cohort. “It is, therefore, conceivable, although speculative, that the association of suicide attempt history with COVID-19 might reflect dysregulated immune function in young and obese attempters, respectively, since individuals with conditions involving immune system dysregulation such as asthma and allergic rhinitis, are more likely to test positive for COVID-19 relative to those without such conditions,” they posited.
The study team also had some recommendations for VA clinicians. They advised that, because of possible long-term neuropsychiatric sequelae of COVID-19 infection, “patients with schizophrenia or schizoaffective disorder who have a history of suicide attempt and are younger than 59 or obese, should be monitored closely since they may be more at risk of COVID-19. Indeed, there is the possibility of symptom exacerbation in patients with a history of suicide attempt who test positive for COVID-19 since postmortem examination of brains of individuals diagnosed with severe COVID-19 infection revealed COVID-19-related impaired brain neurotransmission.”
Their suggestion was that COVID-19 prevention be prioritized and included in the routine care of patients with schizophrenia or schizoaffective disorder who have a history of suicide attempt. As examples, they recommended that mental health providers should routinely educate patients on COVID-19 precautions such as wearing a mask, physical distancing, washing hands and getting vaccinated. Patients also should be informed about COVID-19 symptoms and the importance of seeking medical attention if they experience such symptoms, the authors wrote.
The researchers called for future well-powered, prospective studies to confirm the apparent association between history of suicidal behavior and COVID-19 in patients with schizophrenia or schizoaffective disorder and to better explain the underlying mechanisms that underlie that link.
As of early April 2022, the VA reported that 21,671 COVID-19-related deaths had occurred among its patients since the beginning of the pandemic in March 2020. Cumulative cases overall were nearly 620,000.
- Okusaga OO, Kember RL, Peloso GM, Peterson RE, Vujkovic M, Mitchell BG, Bernard J, Walder A, Bigdeli TB. History of Suicide Attempts and COVID-19 Infection in Veterans with Schizophrenia or Schizoaffective Disorder: Moderating Effects of Age and Body Mass Index. Complex Psychiatry. 2021 Dec 1;392:1789-1795. doi: 10.1159/000521230. PMID: 35128521; PMCID: PMC8805065.