Conventional wisdom has suggested that insulin requirements go down with advanced chronic kidney disease in Type 2 diabetes patients. That does not always appear to be the case, however. A recent study found that patients with both T2D and CKD are at much higher risk of severe hypoglycemia with insulin use.
SALT LAKE CITY — The use of insulin was greater in Type 2 diabetes patients with advanced chronic kidney disease, according to a new study, which also found that both insulin therapy and advanced CKD were independent risk factors for serious hypoglycemic events.
The report in BMC Nephrology pointed out that, compared to patients with preserved kidney function and not on insulin, insulin users who had eGFR < 30 ml/min/1.73 m2 faced a nearly 5.3-fold higher risk of dangerous hypoglycemia.
Researchers from the VA Salt Lake City Healthcare System and the University of Utah Health Sciences sought to determine whether, in general, patients with more advanced CKD and T2D increased their hypoglycemia risk by using insulin.
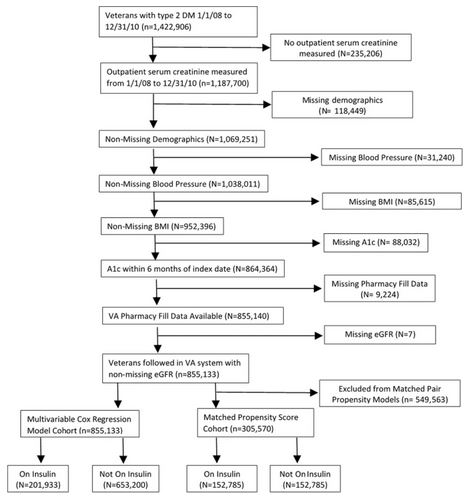
To do that, they analyzed records of a national cohort of 855,133 veterans with T2D seen at VAs clinics between Jan. 1, 2008, and Dec. 31, 2010, with at least two serum creatinine measurements. For purposes of the study, data on insulin use was pulled from pharmacy records and ICD-9/10 codes from emergency room visits or hospitalizations that occurred until Dec. 31, 2016, were searched for evidence of serious hypoglycemic events.
Participants’ mean age was 66 ± 11 years, 97% of them were men, and their mean baseline eGFR was 73 ± 22 ml/min/1.73 m2.
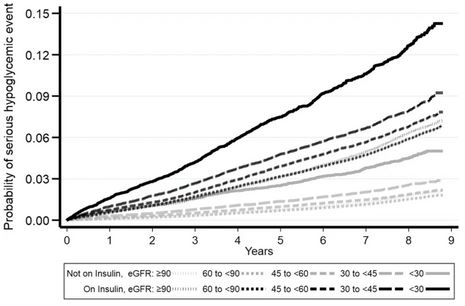
Click To Enlarge: Kaplan-Meier curves for probability of serious hypoglycemic event by insulin and eGFR groups.
Source: BMC Nephrol 23, 73 (2022).
With 653,200 veterans without insulin use at baseline, researchers determined that the eGFR < 30 group had higher hazard (HR 1.80, 95% CI 1.74 to 1.88) of subsequent insulin use compared to eGFR ≥90 group. Using a model with propensity score-matching for baseline insulin use in 305,570 patients, they determined that both insulin use (HR 2.34, 95% CI 2.24 to 2.44) and advanced CKD (HR 2.28, 95% CI 2.07 to 2.51 for comparison of eGFR < 30 to eGFR ≥90 ml/min/1.73 m2 groups) were linked with increased risk of subsequent serious hypoglycemic events.
“In T2D, more advanced CKD was associated with greater insulin use. Both insulin use and advanced CKD were risk factors for serious hypoglycemic events,” the authors concluded. “The safety of insulin compared to newer glycemic agents in more advanced CKD needs further study.”
Background information in the article advised that more than 30 million adults in the United States have diabetes mellitus (DM), which is the leading cause of CKD; nearly 1 in 3 of diabetes patients develop kidney disease.
Yet, according to the article, “Despite the public health importance of kidney disease in persons with Type 2 diabetes (T2D), there is a paucity of data on optimal treatment for glycemic control in this population. Fundamental questions such as the role of insulin in glycemic control in CKD still need to be addressed.”
The researchers pointed out that, while it is often assumed that insulin requirements go down with advanced CKD because insulin is cleared by the kidney, cross-sectional studies indicate higher insulin use in patients with more advanced CKD. “Therefore, it remains unclear whether the need for insulin is decreased or increased in advanced CKD,” they added. A serious adverse effect of insulin therapy is hypoglycemia that results in emergency room visit or hospitalization. While insulin therapy is a known risk factor for hypoglycemic episodes, whether advanced CKD by itself is associated with increased risk of hypoglycemia has been controversial.
A study of veterans more than 10 years ago by the University of Maryland concluded, “CKD is a risk for hypoglycemia, with or without diabetes. The excessive mortality associated with hypoglycemia makes this complication a significant threat to patient safety in CKD.”2
Hypoglycemia Was Common
A prospective observational study that included veterans in 2019 found that, for T2D patients with moderate to severe CKD, hypoglycemia was common, especially with tighter glycemic control. Researchers from Banner-MD Anderson Cancer Center in Houston and colleagues from the VA Puget Sound Healthcare System and other institutions pointed out, however, that their results were not significantly different from groups with similar clinical characteristics and preserved eGFR.3
Each of the 81 participants with CKD wore a continuous glucose monitor for two six-day periods. The study team examined rates of sustained level 1 hypoglycemia (<70 mg/dl) and Level 2 hypoglycemia (<54 mg/dl) among participants with CKD. During the 890 total days of continuous glucose monitoring, participants with CKD recorded 255 episodes of Level 1 hypoglycemia, and 68 episodes reached Level 2.
The authors calculated the median rate of hypoglycemic episodes at 5.3 (interquartile range, 0.0-11.7) per 30 days and mean time spent in hypoglycemia as 28 (SD 37) minutes per day. Compared with control populations, participants with CKD were not observed to have significant differences in time in hypoglycemia (adjusted differences 4 [95% confidence interval, -12 to 20] and -12 [95% confidence interval, -29 to 5] minutes per day), however, the study noted.
The authors of the BMC Nephrology study suggested, “The question of whether both insulin use and advanced CKD are independently associated with increased risk of hypoglycemia may have therapeutic implications for glycemic control in persons with T2D and CKD as hypoglycemic episodes are associated with increased risk of CKD progression, stroke and mortality.”
The researchers suggested several biological explanations for their findings, including that insulin resistance is common in CKD. They said that could be associated with pro-inflammatory cytokines such as interleukin-6 and tumor necrosis factor-⍺ and oxidative stress—all of which might be involved in insulin resistance.
Another possibility, they wrote, is that pancreatic beta-islet cells have low expression of antioxidant enzymes and, as a result, are extremely sensitive to oxidative stress. The authors referred to experimental data positing that beta cell dysfunction might be made worse in CKD because of increased oxidative stress from the accumulation of uremic toxins.
The researchers also pointed out that many of the anti-diabetic medications are contraindicated in advanced CKD, explaining, “Thus, this combination of decreased insulin production, peripheral insulin resistance and contraindications for other medications could increase the need for exogenous insulin for glycemic control in CKD.”
In terms of the apparent link between advanced CKD and higher risk of hypoglycemia, the authors noted that renal gluconeogenesis is essential in countering hypoglycemia in healthy adults.
“People with moderate to severe CKD have reduced kidney mass and therefore, a reduced capacity for glucose release from the kidneys, which might increase the risk for hypoglycemia,” they advised. “However, the previous data on whether CKD is a risk factor for hypoglycemia has been conflicting. Some of the previous studies noted such an association, but not all.”
The study also discussed the dangers of hypoglycemia, which raises the risk of mortality, cardiovascular disease, cognitive impairment and progression of CKD. The authors urged that the “the safety profile of insulin compared to newer glycemic agents such as SGLT-2 inhibitors and GLP-1 analogs in advanced CKD needs to be further examined in randomized controlled trials to determine optimal glycemic control therapy in this population.”
The researchers concluded, “In summary, contrary to widely held assumption that advanced CKD is associated with decreased need for insulin, we found that insulin use was greater in T2D patients with more advanced CKD. Furthermore, this study also found that both insulin use and CKD are independent factors for risk of hypoglycemia, with patients with advanced CKD who use insulin being at the highest risk for a hypoglycemic event. Future randomized controlled trials are needed to determine the safety of insulin compared to newer glycemic agents in patients with T2D and advanced CKD.”
- Grube, D., Wei, G., Boucher, R. et al. Insulin use in chronic kidney disease and the risk of hypoglycemic events. BMC Nephrol 23, 73 (2022). https://doi.org/10.1186/s12882-022-02687-w
- Moen MF, Zhan M, Hsu VD, Walker LD, Einhorn LM, Seliger SL, Fink JC. Frequency of hypoglycemia and its significance in chronic kidney disease. Clin J Am Soc Nephrol. 2009 Jun;4(6):1121-7. doi: 10.2215/CJN.00800209. Epub 2009 May 7. PMID: 19423569; PMCID: PMC2689888.
- Ahmad I, Zelnick LR, Batacchi Z, Robinson N, Dighe A, Manski-Nankervis JE, Furler J, O’Neal DN, Little R, Trence D, Hirsch IB, Bansal N, de Boer IH. Hypoglycemia in People with Type 2 Diabetes and CKD. Clin J Am Soc Nephrol. 2019 Jun 7;14(6):844-853. doi: 10.2215/CJN.11650918. Epub 2019 Apr 17. PMID: 30996047; PMCID: PMC6556736.