Women represented less than 10% of U.S. veterans in 2017, according to the National Center for Veterans Analysis and Statistics, but the number of women veterans receiving VHA care has increased by 22.1%, from 423,642 in 2014 to 517,241 in 2018 and is predicted to burgeon even more in the future. That’s why studies such as one examining the role of estrogen and menopause in glaucoma are so important to the VA.

In 2018, Seth Holst, MD, an ophthalmologist conducted an eye exam at the VA Pittsburgh
Healthcare System. Menopause appears to be a risk factor for glaucoma in older women. VA photo.
ATLANTA — Most, 59%, of the 41.3 million patients worldwide with glaucoma are woman, who, even though they report a higher rate of visual impairment than men, are 24% less likely to seek treatment for the ophthalmologic condition.
That’s according to a study led by the Atlanta VA Healthcare System and Emory University School of Medicine. The authors advised that, based on the data, “glaucoma affects women more severely than men and that the number of affected women remains underreported. Unfortunately, in preclinical research, female animals are frequently omitted, with 75-82% of rodent studies only using male animals. This makes it nearly impossible to identify underlying causes of a disease or responsiveness to drug treatments that may differ between sexes.”
Their report in Cellular and Molecular Neurobiology pointed out, however, that the importance of focusing on sex-based differences in glaucoma concerning disease development, progression and treatment has been underscored by recent funding policies, including the National Institutes of Health (NIH) and Women’s Veterans Health Research Network.
“Thus, in glaucoma the importance of sex has become more relevant,” the authors wrote, “Yet, the effect of sex-specific risk factors in glaucoma is not often considered, likely because sex has not been unequivocally identified as a risk factor for glaucoma.”
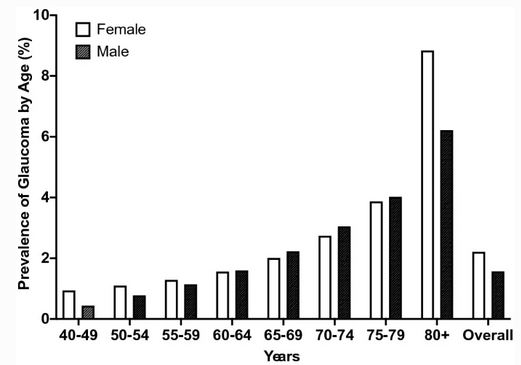
Click To Enlarge: Prevalence of any type of glaucoma by age between males and females by decade. Source: Cell Mol Neurobiol. 2022 Jan 4.
Noting that the National Eye Institute (NEI) recently reported that females in the United States have an overall higher prevalence of all types of glaucoma compared to men—2.21% in females vs. 1.67% in males—researchers said the difference is not fully explained by the usual explanation. That essentially is that longer life expectancies in women led to the overall higher prevalence of glaucoma, which increases with age.
Study authors argued that “the difference in life expectancy cannot fully explain the overall higher prevalence of all types of glaucoma in females, as middle-aged women (ages 40-59) also have a modestly higher prevalence of glaucoma compared to similarly aged men.”
One possible explanation for the difference, they added, is that current epidemiological, clinical and basic science evidence suggest that estrogen plays a role in the aging of the optic nerve. Circulating sex hormones, such as estrogen, decrease with menopause.
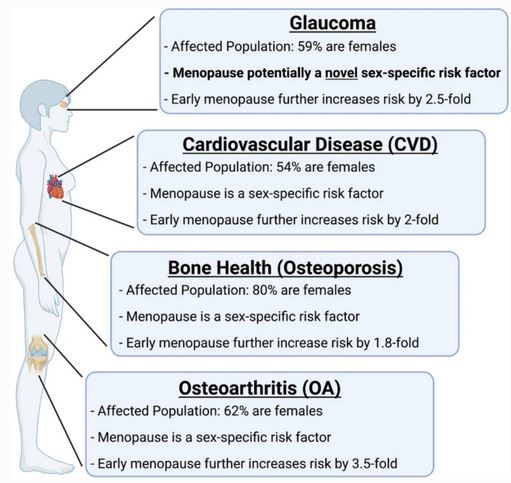
Click To Enlarge: Summary of the pathologies highlighted in this review. Source: Cell Mol Neurobiol. 2022 Jan 4.
That led to an exploration of whether menopause is a sex-specific risk factor for glaucoma. To answer that question, researchers investigated how menopause is defined as a sex-specific risk factor for other pathologies, including cardiovascular disease, osteoarthritis and bone health. Next, they reviewed clinical evidence on the potential role of menopause in glaucoma. They also analyzed preclinical studies that showed greater vision and retinal ganglion cell (RGC) loss following surgical menopause and how estrogen is protective in models of RGC injury. The study team also explored how surgical menopause and estrogen signaling are related to risk factors associated with developing glaucoma, including intraocular pressure, aqueous outflow resistance and ocular biomechanics.
Sex-Specific Factor
The result was the hypothesis that menopause potentially sets the stage to develop glaucoma and therefore is a sex-specific risk factor for this disease.
Some of the same researchers suggested that estrogen deficiency intensifies visual impairment, based on their research with rats. That report, which involved experimental menopause, was published in Experimental Eye Research in 2019.
In the more-recent article, the researchers emphasized that “understanding the impact of menopause on glaucoma and retinal ganglion cell survival has potential clinical applications in the management of glaucoma. Further, as estrogen is known to be neuroprotective, it may potentially have a role in the treatment of non-glaucomatous optic neuropathies, such as ischemic optic neuropathy, compressive optic neuropathy, and traumatic optic neuropathy.”
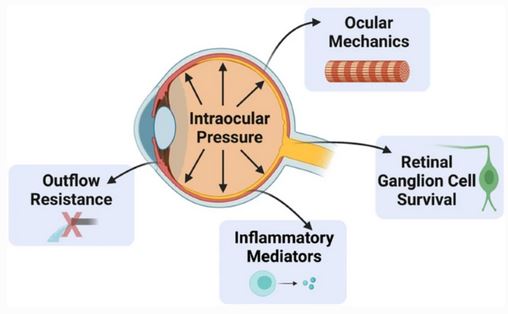
Click To Enlarge: Illustration of how menopausal status and estrogens influence properties throughout the eye. Several of these are direct risk factors for developing glaucoma (e.g., increasing IOP and outflow resistance and decreasing ocular stiffness). Source: Cell Mol Neurobiol. 2022 Jan 4.
The authors added, “The association of menopause and its relationship to glaucoma has an ever-growing body of literature. The similarities of menopause (or ovariectomy) in glaucoma with other major pathologies build a foundation that menopause, a major life event in women, may be a sex-specific risk factor for glaucoma development and/or progression. Further, in ocular research the consistency across laboratories, animal models, and various injury models supports the idea of menopause as a sex-specific risk factor for developing glaucoma that warrants more attention.”
The findings are especially significant for VA healthcare providers. Women represented less than 10% of U.S. veterans in 2017, according to the National Center for Veterans Analysis and Statistics, but the number of women veterans receiving VHA care has increased by 22.1%, from 423,642 in 2014 to 517,241 in 2018, according to a report last year in Women’s Health Issues.
“Looking forward, the VHA anticipates this population will continue to increase, from 9.4% of the U.S. veteran population in 2015 to 16.3% of the U.S. veteran population by 2043,” wrote the authors from the VA Northeast Ohio Healthcare System in Cleveland and colleagues. “Since 2006, the VHA has increased attention to gender differences in quality and performance measures to identify gaps in women veterans’ quality of care, respond to the needs of the growing women veteran population, and decrease gender health disparities.”
- Douglass A, Dattilo M, Feola AJ. Evidence for Menopause as a Sex-Specific Risk Factor for Glaucoma. Cell Mol Neurobiol. 2022 Jan 4. doi: 10.1007/s10571-021-01179-z. Epub ahead of print. PMID: 34981287.
- Feola AJ, Fu J, Allen R, Yang V, Campbell IC, Ottensmeyer A, Ethier CR, Pardue M. Menopause exacerbates visual dysfunction in experimental glaucoma. Exp Eye Res. 2019 Sep;186:107706. doi: 10.1016/j.exer.2019.107706. Epub 2019 Jun 18. PMID: 31226338; PMCID: PMC6900868.
- Marshall V, Stryczek KC, Haverhals L, Young J, Au DH, Ho PM, Kaboli PJ, Kirsh S, Sayre G. The Focus They Deserve: Improving Women Veterans’ Health Care Access. Women’s Health Issues. 2021 Jul-Aug;31(4):399-407. doi: 10.1016/j.whi.2020.12.011. Epub 2021 Feb 10. PMID: 33582001.

