VHA’s 6% Rate in Line With Other US Healthcare Systems
Colonoscopy might be one of the best tools for detecting colorectal cancer, but that doesn’t mean it’s foolproof. Some cases of CRC are missed, usually because they are too small to detect. The VHA’s 6% rate of post-colonoscopy CRCs is in line with other U.S. healthcare systems and is an indicator of a high-quality CRC screening program, according to a new study.
INDIANAPOLIS — Although colonoscopy is considered a gold standard for the detection and prevention of colorectal cancer (CRC), some patients are diagnosed with CRC even when nothing concerning was identified during the screening.
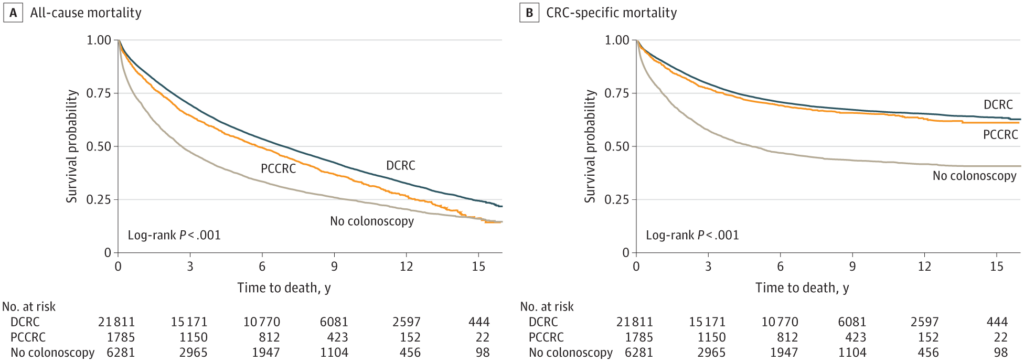
Click to Enlarge: Kaplan-Meier Curves for All-Cause and Colorectal Cancer (CRC)–Specific Mortality Source: JAMA Network Open
Within the VHA, according to a new study, about 6% of veterans were diagnosed with CRC after a colonoscopy that did not diagnose cancer but prior to the next guideline-recommended examination. The VA healthcare system diagnoses about 4,000 cases of colon cancer every year among its veteran patients.
“These post colonoscopy CRCs (PCCRCs) reflect the quality of the index colonoscopy and are considered a barometer of colonoscopy quality at the institutional and health care system levels,” wrote researchers from the Richard L. Roudebush VAMC, Indiana University School of Medicine and The Regenstrief Institute, all in Indianapolis. “Most PCCRCs are attributed to missed or incompletely resected colorectal lesions (CRC or precancerous polyps), whereas fast-growing tumors account for a small proportion of PCCRCs.”
The study in JAMA Network Open also pointed out that the variability in effectiveness of colonoscopy might be attributed to operator-dependent factors, which is “critical because these factors are potentially remediable with educational and quality improvement initiatives.”1
The study team sought to examine PCCRC prevalence and its all-cause mortality (ACM) and CRC-specific mortality (CSM) within the VA healthcare system. To do that, researchers conducted a retrospective cohort study using VA-Medicare administrative data to identify 29,877 veterans aged 50 to 85 years with newly diagnosed CRC between Jan. 1, 2003, and Dec. 31, 2013, with final analysis in September 2022.
For purposes of the study, they categorized patients whose colonoscopy occurred less than 6 months before CRC diagnosis with no other colonoscopy within the previous 36 months as having detected CRC (DCRC). Those who had a colonoscopy that did not detect CRC between 6 and 36 months before CRC diagnosis were categorized as having post-colonoscopy CRC (PCCRC-3y). An additional group included patients with CRC and no colonoscopy within the prior 36 months.
Participants had a median age of 67, and 98% were male. Most, 80%, were white, with 18% Black veterans and 2% categorized as other. While 6% were classified as having PCCRC-3y, the vast majority, 73%, were considered to have DCRC.
The 5-year all-cause-mortality rates were 46% vs. 42% for patients with PCCRC-3y and DCRC, respectively. Patients with PCCRC-3y had 5-year CSM rates of 26% compared to 25% for patients with DCRC.
“In multivariable Cox proportional hazards regression analysis, there was no significant difference in ACM and CSM between patients with PCCRC-3y (adjusted hazard ratio [aHR], 1.04; 95% CI, 0.98-1.11; P = 0.18) and patients with DCRC (aHR, 1.04; 95% CI, 0.95-1.13; P = 0.42),” the authors wrote. “However, compared with patients with DCRC, patients with no prior colonoscopy had significantly higher ACM (aHR, 1.76; 95% CI, 1.70-1.82; P < 0.001) and CSM (aHR, 2.22; 95% CI, 2.12-2.32; P < 0.001). Compared with patients with DCRC, patients with PCCRC-3y had significantly lower odds of having undergone colonoscopy performed by a gastroenterologist (odds ratio, 0.48; 95% CI, 0.43-0.53; P < 0.001).”
Mortality Rate Not Affected
Overall, the study found that rates of PCCRC-3y in the VA system was similar to other settings and that having PCCRC-3y didn’t have much effect on ACM and CSM, compared with other CRC patients.
The researchers also reported that, compared with patients with DCRC, those with PCCRC-3y had comparable cancer stage distribution, higher predilection for proximal colon location and increased risk of a medically urgent presentation, such as bowel obstruction or peritonitis. “Performance of colonoscopy outside the VA was associated with PCCRC-3y but not with mortality,” they noted.
In line with previous studies indicating that endoscopist specialty is a factor associated with colonoscopy quality, the study determined lower odds of PCCRC-3y when procedures were performed by gastroenterologists.
Background information in the report noted that past research has estimated prevalence rates of PCCRC-3y that range from approximately 2% to 10% of all CRC cases and a predilection for the proximal colon.
In the VHA, one of the largest integrated healthcare systems in the United States, colorectal cancer screening “is widely practiced and is guided by directives that emphasize the importance of high-quality screening and require measurement and reporting of colonoscopy quality metrics,” the authors pointed out.
“Measuring and monitoring the rates of PCCRC and its associated factors and consequences for patient outcomes is critical to meaningful quality improvement and ensuring that veterans receive high-quality colonoscopies,” the study added. “In addition, studying PCCRC in the VHA has broad relevance, which extends beyond the confines of a single healthcare system. Given its size and the fact that the VHA serves as a reference standard in the health care field, the knowledge derived from a VHA-based study can help inform patients, practitioners, and policy makers in other health care organizations and enrich the CRC research field as a whole.”
As to why PCCRC occurs, the study team noted that most cases occur because most of these cancers are still small and at an early stage within a 3-year interval after colonoscopy. “The observation that patients with DCRC and patients with PCCRC-3y had similar cancer stage distribution supports this notion and is consistent with a dwell time for PCCRC-3y similar to that of sporadic DCRC,” they advised. “In turn, this finding supports the notion that accelerated neoplasia progression may not be a major factor in the pathogenesis of most PCCRC”
Also of note is that the study determined that patients with CRC and no prior colonoscopy had significantly worse ACM and CSM than either PCCRC-3y or DCRC. “This finding is likely driven by the fact that nearly 40% of patients in this group had stage IV cancers at diagnosis, compared with 15% to 17% in the other two groups,” the researchers wrote. “This observation is not surprising because patients who recently underwent colonoscopy are expected to benefit from the detection of cancer in its early stages and from CRC prevention via polypectomy.”
The study also pointed out that 93% of patients in the no colonoscopy group had undergone colonoscopy more than 10 years before CRC diagnosis or had no colonoscopy that could be identified in the Corporate Data Warehouse or CMS data. The authors emphasized that their finding puts a spotlight on the importance of regular and programmatic CRC screening and of measuring colonoscopy quality.
- Kahi CJ, Myers LJ, Monahan PO, Barker BC, Stump TE, Imperiale TF. Mortality After Postcolonoscopy Colorectal Cancer in the Veterans Affairs Health Care System. JAMA Netw Open. 2023;6(4):e236693. doi:10.1001/jamanetworkopen.2023.6693
