Among the most complex patients treated in the VA healthcare system are those with serious mental illnesses, including the more than 120,000 diagnosed with schizophrenia. Those patients not only tend to have worse physical function as they age, but also are more likely to engage in suicidal behavior. To better understand what increases the risk of schizophrenia and other serious mental illnesses, VA researchers are taking a close look at social determinants of health.
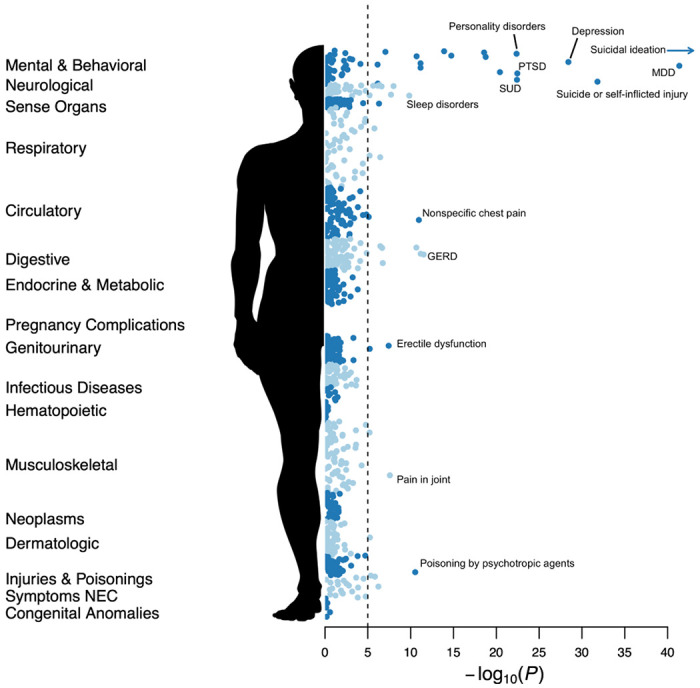
Click to Enlarge: PheWAS for suicidality phenotypes in CSP #572. PheWAS results for suicidal behaviors across 1,000 disease categories. The dotted line indicates an approximate Bonferroni adjusted p-value threshold for the number of Phecodes tested. Source: The National Library of Medicine
SAN DIEGO — Schizophrenia and other serious mental illnesses put veterans at higher risk of suicidal behavior and significantly compromise the physical health of older VHA patients. That’s why VA researchers are seeking to better understanding the causes of schizophrenia-spectrum psychotic disorders (SSPD).
More than 120,000 veterans receiving VHA care have been diagnosed with schizophrenia, according to 2014 study.1
One promising area of study is social determinants of health (SDoHs). A new study involving VA researchers from San Diego and Miami performed a scoping review of meta-analyses and systematic reviews of nine major SDoHs in SSPD. An impetus was SSPD patients’ “heightened risk of comorbidities, cognitive and functional decline,” according to the authors.
The study in the Schizophrenia Bulletin found the following to be major risk factors for the greater incidence of SSPD, as well as worse health:2
- childhood abuse,
- parental psychopathology,
- parental communication problems,
- bullying, and
- urban settings with lower socioeconomic status.
On the other hand, social network size was inversely associated with overall psychopathology and negative symptoms.
“Experiences of racial/ethnic discrimination correlated with the prevalence of psychotic symptoms and experiences. Compared to native populations, the risk of psychosis was higher in immigrants, refugees and asylees,” the authors wrote.
The study also found that schizophrenia was increasingly prevalent with social fragmentation, and that homeless populations had a 30-fold higher prevalence of schizophrenia than the general population. Among the prison population, the prevalence of nonaffective psychosis was 2.0%-6.5%, compared to 0.3% in the general population.
The consequences could be dire, the authors wrote, with seriously mentally ill people 2.7 times more likely to report food insecurity than controls.
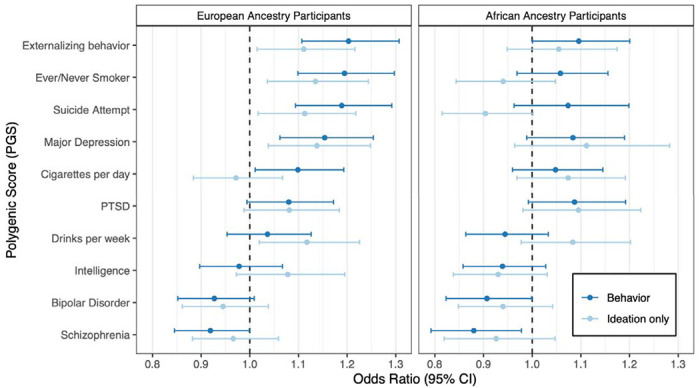
Click to Enlarge: Associations of PGS with suicidality behaviors in SCZ and BPI. For each polygenic score, the odds ratio (per unit increase) corresponding to the best-performing P-value threshold is shown. Displayed results are based on the EA cohort, and adjusted for diagnosis, sex, and age. Source: The National Library of Medicine
“SDoHs are associated with higher rates of and worse outcomes in SSPD,” the authors wrote. “Well-designed longitudinal studies are needed to understand SDoHs’’ contribution to health in persons with SSPD, to develop interventions, and to implement changes in clinical care and public health policies that would reduce adverse health impacts of SDoHs. Positive SDoHs deserve greater attention.”
Self-Injurious Behavior
A recent VA study appearing as a preprint prior to publication pointed out that patients diagnosed with schizophrenia (SCZ) or bipolar I disorder (BPI) are at high risk for self-injurious behavior, suicidal ideation and suicidal behaviors (SB). “Characterizing associations between diagnosed mental and physical health problems, prior pharmacological treatments, and aggregate genetic factors has potential to inform risk stratification and mitigation strategies,” the study team wrote.3
Researchers focused on 3,942 SCZ and 5,414 BPI patients receiving VA care. They assessed self-reported SB and ideation using the Columbia Suicide Severity Rating Scale (C-SSRS). The cross-sectional data were integrated with electronic health records (EHR), and compared by lifetime diagnoses, treatment histories, follow-up screenings, and mortality data. Available genomic data were used to construct polygenic scores (PGS) for traits related to psychiatric disorders, substance use, and cognition, while exploratory genomewide association studies were performed to identify and prioritize specific loci.
The study pointed out that only 20% of veterans who self-reported SB had a corroborating ICD-9/10 code in the electronic health record. In addition, more than 20% of veterans who denied prior behaviors reported new-onset SB at follow-up.
“SB were associated with a range of psychiatric and non-psychiatric diagnoses, and with treatment with specific classes of psychotropic medications (e.g., antidepressants, antipsychotics, etc.),” the researchers advised. “PGS for externalizing behaviors, smoking, suicide attempt, and major depressive disorder were also associated with attempt and ideation.”
While the authors said they didn’t find any significant loci among individuals with a diagnosed mental illness, self-reported SB were strongly associated with clinical variables across several areas.
“Overall, clinical and polygenic analyses point to sequelae of substance-use related behaviors and other psychiatric comorbidities as strong correlates of prior and subsequent SB,” the study concluded. “Nonetheless, past SB was frequently not documented in clinical settings, underscoring the value of regular screening based on direct, in-person assessments, especially among high-risk individuals.”
Serious mental illness also has a detrimental effect on physician function of veterans, according to another recent study.
A study led by the VA Providence, RI, Healthcare System and the Alpert Medical School of Brown University sought to characterize the physical function of older veterans with serious mental illness (SMI) across endurance, strength and mobility domains.
The retrospective analysis of clinical performance data focused on participants in the VHA’s Gerofit program, a national outpatient supervised exercise program for older veterans. Included were 166 veterans aged 60 and older with SMI and 1,441 without who were enrolled in eight national Gerofit sites between 2010 and 2019. Results were published in the American Journal of Geriatric Psychiatry.4
Researchers assessed performance measures of physical function covering endurance (6-minute walk test), strength (chair stands, arm curls), and mobility (10-meter walk, 8-foot-up-and-go) administered at Gerofit enrollment. The goal was to construct functional profiles of older veterans with SMI compared to other veterans.
Results indicated that older veterans with SMI performed worse on all measures of function, including chair stands, arm curls, 10-meter walk, 6-minute walk test, 8-foot-up-and-go, compared to age- and sex-based reference scores with statistically significant differences present in the male sample. “Functional performance of those with SMI was also worse compared to propensity-score matched older veterans without SMI with statistically significant differences on chair stands, 6-minute walk test, and 10-meter walk,” the authors wrote.
The study concluded that older veterans with SMI have compromised strength, mobility and endurance. The authors urged that physical function be a core component of screening and treatment for this population.
- Sun F, Stock EM, Copeland LA, Zeber JE, et. al. Polypharmacy with antipsychotic drugs in patients with schizophrenia: trends in multiple health care systems. Am J Health Syst Pharm. 2014 May 1;71(9):728-38. doi: 10.2146/ajhp130471. PMID: 24733136; PMCID: PMC4432466.
- Jester DJ, Thomas ML, Sturm ET, Harvey PD, et. al. Review of Major Social Determinants of Health in Schizophrenia-Spectrum Psychotic Disorders: I. Clinical Outcomes. Schizophr Bull. 2023 Apr 6:sbad023. doi: 10.1093/schbul/sbad023. Epub ahead of print. PMID: 37022779.
- Bigdeli TB, Barr PB, Rajeevan N, Graham DP, et. al. Million Veteran Program (MVP); Cooperative Studies Program (CSP) #572; Huang GD, Concato J, Siever LJ, DeLisi LE, Kimbrel NA, Beckham JC, Swann AC, Kosten TR, Fanous AH, Aslan M, Harvey PD. Correlates of suicidal behaviors and genetic risk among United States veterans with schizophrenia or bipolar I disorder. medRxiv [Preprint]. 2023 Mar 8:2023.03.06.23286866. doi: 10.1101/2023.03.06.23286866. PMID: 36945597; PMCID: PMC10029042.
- Browne J, Elbogen EB, Mueser KT, Rudolph JL, et. al. Physical Function Assessment of Older Veterans With Serious Mental Illness. Am J Geriatr Psychiatry. 2023 Mar 2:S1064-7481(23)00235-X. doi: 10.1016/j.jagp.2023.02.048. Epub ahead of print. PMID: 36941144.
